-


Horizontal Ridge Augmentation
Ridge augmentation is sometimes needed to establish proper soft and hard tissue support before placing a dental implant. The horizontal augmentation procedure is commonly used in dental clinics to restore bone defects in people with destructive gum disease. There are many variables to investigate to optimize these treatments, for which several animal models exist. Defects can be created surgically in skeletally mature animals to study changes over time. The site of both defects and implants can also be varied, and the merits of staged or simultaneous tooth extraction and insertion of implants can be evaluated. Different types of graft material (block, particulate or autogenous), bone fillers and bone substitutes can be applied, and resorbable and non-resorbable, natural and synthetic membranes can also be compared. A major aim of these studies is to identify procedures and materials giving the most predictable outcomes. The chapter describes valid endpoints evaluated by histomorphometry, specific staining techniques, and a host of imaging modalities. It also covers other aspects of successful, reproducible experiments, such as planning, report writing, ethical approval, funding applications and submission, with the overall aim of producing new, safe clinical innovations that rapidly restore quality of life to patients. -

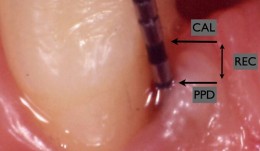
Examiner Standardization And Calibration
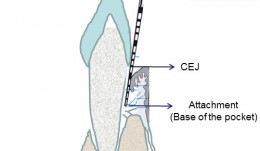
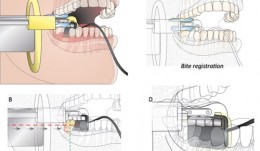
based on the book chapter by Hatice Hasturk and Mary Ann Cugini Summary The emphasis of this chapter is on examiner--therapist alignment and standardization when conducting controlled clinical trials, especially those with multicenter settings. It begins with definitions of various key research team members and follows by giving specific advice on assessing regeneration by periodontal and bone probing, with reference to parameters relating to probing depth, the cemento--enamel junction, gingival margins, keratinized gingiva, tooth mobility, clinical attachment and alveolar bone gain. The authors explain the relevance of bleeding, plaque and gingival health indices, and the stress the importance of selecting suitable reference points and scoring scales. Detail is provided on the techniques of mucogingival regeneration, alveolar ridge augmentation and implant insertion, and factors such as wound healing. There are protocols for alignment and agreement sessions, and recommendations for conducting regular realignment sessions, with tailored training and calibration, in order to ensure consistency in skills and performance of the team, in data capture and interpretation, and in use of instruments and scoring systems. Practical tips are given on various aspects of the study including set up and timings, examiner--observer agreement and inter-class correlation, with guidance on organizing the research team, assessment plans and statistical analysis. The overall aim of the chapter is to ensure production of high-quality data with minimal uncertainty. Open full-text PDF (1.4 MB) -


Statistical Analysis
based on the book chapter by Jrg Hsler Summary This chapter will enable clinical investigators to select statistical methods that extract results and conclusions from quantitative data which are both meaningful and can be compared with findings of other studies. Among the key issues discussed are the need to develop a data analysis plan, to engage a biostatistician early in the design process, and to conduct a power analysis to determine how many participants should be recruited and how many to include in treatment and control groups. There are explanations of different types of randomization processes (simple, stratified, balanced or computer-generated), error probabilities and error corrections, data distribution, and rejection of the null hypothesis on the basis of a statistical test decision. The authors explain how to choose suitable endpoints and analytical tools for specific clinical scenarios that relate to the study hypothesis. The role of descriptive measures, statistical estimates and graphs is made clear, including the concepts of confidence intervals, means, medians and standard deviations. They also describe how statistical models such as analysis of variance (ANOVA) are used to explore relations between variables, and one-way and two-way tests are used to explore relations between impact factors. The role of multiple testing is clarified, and the use of Tukey and Bonferroni corrections, Newman--Keulbs, Scehhe and Dunn devices, and Fishers least significant device (LSD) in error correction. Open full-text PDF (1.1 MB) -

Analytical Methods: Histology
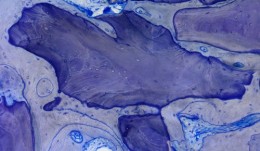
based on the book chapter by Dieter D. Bosshardt Summary Histological assessment, which can be quantitative or qualitative, is an indispensable tool for investigation of soft tissue regeneration. Harvesting tissues raises ethical considerations, but less invasive forms of evaluation, such as clinical measures and imaging, only complement the descriptive analysis, rather than replace it, by showing how cells respond to biomaterials in vivo. This chapter explores various methods for evaluating hard and soft oral tissues, such as histomorphometry, in situ hybridization and autoradiography, in the context of procedures like socket preservation, ridge augmentation and sinus floor elevation. As well as outlining suitable endpoints and landmarks, it discusses tools and techniques for taking biopsies, cutting, sectioning and embedding samples, and the use of microscopy and illumination. The authors address the challenges posed by different biomaterials -- not all can be sectioned, and some react with the chemicals used for processing samples. Thus tissue sections may be of unpredictable quality and be affected by artifacts introduced before fixation (if the tissue gets crushed during harvesting or contaminated by oral pathogens) or during fixation or preserving. Other challenges include the acquisition, processing, analysis and storage of digital images, and the huge variations in analytical equipment and methods used in different laboratories, where the need to apply laboratory standards and minimize examiner variation is emphasized. Open full-text PDF (1.9 MB) -

Analytical Methods: Imaging
based on the book chapter by Erika Benavides and Hector F. Rios Summary Clinical imaging allows qualitative and quantitative assessment of hard and soft oral tissues in patients after procedures such as ridge augmentation. This comprehensive guide deals with in vivo and ex vivo and intraoral and extraoral methods. It covers standardized digital intraoral radiography, cone beam (CBCT) and multislice (MSCT) computed tomography, subtraction radiography, ultrasound, optical coherence tomography (OCT), and newer methods such as CAD/CAM (computer-aided design/computer-aided manufacturing) and fractal analysis. There are descriptions on how each modality words, and outlines of their common applications, relative merits and limitations. Among the issues addressed are wave type (e.g infrared versus ionizing radiation), signal noise, distortion, mage resolution, field of view, scanning time, patient trauma and artifacts such as beam-hardening. Illustrations are used throughout to clarify the discussion. The authors point out which methods are preferable for macrostructure, and which for microstructure; for mineralized tissues, and which for soft tissue contours. Some are better for revealing the functions and dynamics of tissues or volumetric changes; some are better at 3-D visualizations and complex typography; some involve exposing patients to ionizing radiation. The authors stress the importance of integrating information from different modalities (such as CAD/CAM with CBCT) and from different time points, to optimize information available for interpretation. Open full-text PDF (1.8 MB) -


Analytical Methods: Biomarkers And Molecular Biology
based on the book chapter by Alpdogan Kantarci Summary The focus of this chapter is on the range of biomarkers used currently in orodental research at both laboratory and chairside levels. With definitions of what they are, the many different types (ranging from immune factors and hormones to genetic material of disease-causing bacteria and patients) and how they relate to surrogate markers and determinants, it explains how they provide dynamic, specific and accurate measures of disease status, that can be used to supplement information gained from conventional analytical methods. However, the chapter points out their enormous potential for predicting and diagnosing disease, for profiling patient risk, identifying deviations from healthy (before clinical manifestations occur), improving clinical decision-making and facilitating personalized therapy. Drawing on studies of wound healing and regenerative therapies, the authors describe various molecular methods including immunoassays, mass spectrometry, cell cultures, PCR-based assays and newer breakthroughs such as checkerboard hybridization. They review current areas of research into costs, processing time, and normal levels in various tissues (e.g. crevicular fluid, plaque and saliva) in addition to how they vary with individual factors such as gender, ethnicity and age. In clinical trials, cross-sectional longitudinal study designs and integration of clinical and laboratory data are recommended to deal with the complexities of orodental disease. Open full-text PDF (1.2 MB) -


Analytical Methods: Non-Invasive
based on the book chapter by Niklaus P. Lang, Jie Han, andChristina Sim Summary Evaluations of osseointegration in the first few weeks after implant placement may reveal that biologically bonded tissue is still mechanically unstable. There is no standard procedure for assessing primary stability, but this chapter reviews progress with a non-invasive technique known as resonance frequency analysis (RFA). This is sensitive to certain aspects of the boneimplant interface and is quantified as the implant stability quotient (ISQ) which, when measured over time, indicates the extent of bone anchorage. The authors explore the relation between ISQ values and bone characteristics, bone volume density and bone trabecular connectivity, referring to controlled longitudinal clinical studies using the new Osstell mentor instrument and Straumann implants to illustrate their reproducibility and reliability, and providing a range of normative values at which healing is established in different bones in terms of homeostasis and implant stability. The authors also refer to a study that has calculated a drop in ISQ value of a specific magnitude that represents a loss of stability. The ISQ is affected by variations in morphologically different bones and the width, length and surface configuration of implants; it is not affected by implant diameter and surface modification, or instrument position. An in vitro comparison with removal torque and axial load response is also described, whereby RFA is the only method capable of detecting changes in both bone density and cortical thickness. Open full-text PDF (1.3 MB) -


Analytical Methods: Volumetric Measurements
based on the book chapter by David Schneider andSven Mhlemann Summary Volumetric measurements are used to detect changes in tissue dimensions in procedures such as ridge preservation and bone augmentation, and to determine tooth wear and the effects of orthodontic treatment, by converting linear dimensions into three-dimensional volumes. Both clinical and post-clinical methods are covered here. The first method comprises a single fast, simple and low-cost step that gives chairside results. Probes, endodontic files, catheters and tooth-supported stents are used to map surface topography through measures of papillary and alveolar ridge height and soft tissue thickness, among others. Reading and rounding errors may occur, however, or inconsistencies in technique, and some sites may require surgical access. Post-clinical analysis involves taking photographs, impressions, radiographs optical scans for analysis later. The authors explain how volumes are calculated from pixel or voxel counts in specified areas, and the merits of comparing approximate, absolute or relative volumes over time. Labside data can be analyzed in various ways, by different examiners, and stored for a long time. Image quality and magnification can be adjusted. Errors may occur while taking casts or processing and digitalizing data, converting file formats or superimposing datasets. The authors emphasize the need to standardize file formats, reference points, areas of interest and directions, and choose sites that are stable over time, and to calibrate all method and examiners before study startup. Open full-text PDF (1.1 MB) -

Analytical Methods: Assessment Of Esthetics And Color
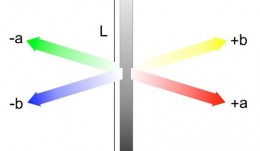
based on the book chapter by Goran Benic and Irena Sailer Summary The visual appearance obtained after tissue reconstruction is an increasingly important aspect of orodental treatment, and hence of research. The esthetic aim is to achieve visual harmony between original and constructed elements. With a focus on metric assessment, the chapter offers guidance on the assessment of soft tissue levels and color matching, describing the scope and uses of ranking systems like the Copenhagen Index, Papilla Index and Implant Crown Esthetic Index, and the Pink/Pink and White Esthetic Scores. It describes how the common systems relate to different types of tissue and their optical, dimensional and surface characteristics, such as mucosal depth. While color match can be assessed using the naked eye, the growing demand for calibration and standardization makes electronic color analyzers more suitable, such as spectrophotometers, that use spectral analysis and CIE-Lab color coordinates and can be calibrated. Discussions cover all clinical parameters of interest and the factors that influence color match with the reconstruction material, such as mucosal thickness. The authors point out the need to make comparisons against healthy natural sites in the same patient, to standardize methods, minimize observer variations and ensure blind assessment. They also discuss how and when to establish baseline values to chart changes, and suggest suitable statistical analyses, with a view to publishing results the can be compared with relevant studies. Open full-text PDF (1.1 MB) -


Study Protocols: Periodontal Regeneration
based on the book chapter by Pierpaolo Cortellini Summary This chapter relates to regeneration of intrabony defects, presenting a protocol that is designed to enhance clinical success rates by standardizing all aspects of the studies in this area surgical approaches, skills and training, calibration of materials and investigators, and defect morphology and patient factors. The design is for a randomized parallel group controlled trial with two treatment arms, both using combination therapy: the test group receives a modified papilla preservation technique (MPPT) plus bovine mineral material and a collagen membrane; the control group receives MPPT plus flap surgery without biomaterials. The biomaterials prevent soft tissue collapse into the defect, and the surgical flaps protect the treated area and reduce wound failure. A suitable number of patients with severe periodontitis is calculated, with recruitment advised through multiple centers. Photographs are provided of the entire surgical procedure from probing to flap closure. The timeline comprises up to 60 days pre-trial workup and 3-monthly post-surgical evaluations for a year to assess all structural and functional changes. The clinical assessments required relate to both molecular and cellular changes (e.g. plaque score, pocket depth, gingival margin and coronal papilla position) and the authors suggest methods for reporting adverse events and obtaining patient-reports, including their quality of life. The protocol recommends construction of generalized linear models as part of the data analysis. Open full-text PDF (1.5 MB) -

Patient-Reported Outcome Measures
based on the book chapter by Colman McGrath Summary There has been a surge of interest in patient-reported outcome measures (PROMs) in all areas of clinical research. Assessing the patients own perceptions of their health, quality of life, functional ability and experience of pain provides very valuable information on the success of an intervention. This chapter describes the development of some commonly used instruments, and summarizes their limitations and suitability for different studies in implant surgery and tissue regeneration. It advises investigators on the selection of different types generic, condition-specific, dimension-specific and utility measures. The authors explain why general (global) instruments like the popular Short Form SF-36 questionnaire have limited sensitivity for oral outcomes, suggesting several condition-specific tools that yield far more specific data and are quick to complete, making them suitable for studies in busy clinic settings and large numbers of patients. The authors describe the role of health utility indexes, which allow patients to rank the importance of items affecting their quality of life, or permit costbenefit analysis of an intervention. The instruments are discussed in the context of their appropriateness for a particular study, their acceptability to patients, validity, reliability and reproducibility, and their responsiveness to change. In terms of interpretation, emphasis is placed on the challenge of identifying the minimally clinically important difference (MCID). Open full-text PDF (0.9 MB) -

Endpoints In Oral And Maxillofacial Regeneration Clinical Trials
based on the book chapter by Mariano Sanz and Fabio Vignoletti Summary Selection of endpoints, or outcome measures, can be daunting for researchers because of the huge variation in disease processes and outcomes relating to implants, surgery and tissue regeneration, and factors such as the research question and study design. This chapter advises investigators on the selection of valid, patient-applicable, sensitive, specific, ethical endpoints, that do not damage tissue integrity. It defines the terms, and distinguishes between true and surrogate and primary and secondary endpoints. It explains about different types biological, clinical, psychological and economic -- and summarizes their limitations and value, such as biological measures for disease etiology and progress, and clinical measures for assessing survival and function. The authors focus on common parameters relating to periodontal probing, bone radiography and patient-related outcomes, and describe the relevance of numerous specific endpoints in studies of localized gingival recession, soft tissue augmentation and mandibular furcation regeneration. They also review endpoint selection in implant therapy, for evaluating bone regenerative therapies, protocols for socket preservation and immediate implantation, lateral and vertical bone augmentation, and implant-supported restorations. Throughout the chapter, the chosen endpoints are related to the wider aspects of patient selection, randomization and compliance, data collection and observer variation, error proneness and reporting of results. Open full-text PDF (2.3 MB)










