-

Clinical and radiografic evaluation with 5 years follow-up of two dental implant-supported mandibular overdentures in the patient receiving oral bisphosphonate therapy
Objectives: Systemic diseases may affect oral tissues by increasing their susceptibility to other diseases or by interfering with healing. Oral bisphosphonates (BP) are commonly prescribed for patients with osteoporosis to arrest bone loss and preserve bone density. The American Association of Oral and Maxillofacial Surgeons (AAOMS) have suggested a cautious approach to implant surgery and extractions for patients receiving bisphosphonate therapy. Methods: Two dental implants (NucleOSS, TR) were inserted in the mandible of a 78-year-old female. The patient has been taking oral alendronate (Fosamax®, marketed by Merck) as a treatment of postmenopausal osteoporosis disease, during the last 3 years. The dose of the bisphosphonate was one tablet of 70 mg once a week. Results: Dental implants in the patient was successful with uneventful healing. There is was no differences between baseline and 5-year Examinations at Recall in PPD, BOP, Mobility, and bone loss. Conclusion: History of oral BP use is not an absolute contraindication for dental implant placement and dental implants can be osseointegrated successfully in this patient population. Great attention should be paid to the regular dental recall for implant-prosthetic restorations. -
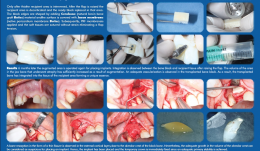

ACHIEVING A MORE EFFICIENT CONTACT SURFACE BETWEEN A BLOCK BONE AND RECIPIENT AREA USING A 3D STEREOLITHOGRAPHY (SLA) MODEL OF A JAW FRAGMENT IN ADJUSTING A HUMAN BONE BLOCK TO THE RESIPIENT AREA AND TIME SAVING DURING OPERATION
Objectives: Autogenic and allogenic bone block materials of different companies are increasingly used in guided bone regeneration (GBR) procedures. Adjusting block-shaped allogenic transplants to fit the recipient area is time consuming and technically challenging. A method of bone block formation using a 3-D stereolithography (SLA) model is reported here. Methods: A tomographic image of the area for augmentation was obtained and edited using Implant Assistant. Data from the image of the prepared 3-D jaw model were transferred to a 3-D printer (Objet Stratasys to produce a model of the jaw fragment. Unicortical cancellous block (Maxgrapht cortico-spongiosa) was moulded onto the model and holes for fixation screws were drilled into the material. The bone block was added to a 100-grams syringe filled with serum, emptied out in to a container and refilled. This procedure was repeated several times. After raising a flap, the recipient area was decorticated and the prepared block put in place. The edges were shaped by adding natural bovine bone graft (Cerobone) material and the surface was covered with native pericardium membrane (Jason membrane). A platelet-rich fibrin (PRF) membrane was then applied and the soft tissues sutured without strain to avoid flap tension. Results: After 6 months, the augmented area was re-operated for implant placement. Integration was observed between the bone block and recipient tissue after raising the flap. The volume of jaw atrophied bone had increased as a result of augmentation. There was adequate vascularisation of the transplanted bone block, which was integrated into the tissue of the recipient area. Bone resorption in the form of a thin fissure was observed in the external cortical layer, close to the alveolar crest of the block. Nevertheless, the growth in alveolar crest volume was deemed adequate for implant placement. A temporary crown was fixed immediately after placement because there was adequate stability, and alveolar crest defect was re-grafted with Cerabone and covered with Jason membrane before the flap was closed. After 4 months, an image was taken that showed bone augmentation and osseointegration around the implant. Conclusions: Preparing a jaw bone fragment as an allogenic bone block using an SLA model done successfully in GBR-type surgeries. The method allows block bone to be adapted for the recipient area, and is associated with significant time savings. Post-operative tomographic scans confirm augmentation of the alveolar ridge, making this a promising way for restoring aesthetics in the frontal area. -


ENAMEL MATRIX DERIVATIVE (EMD) IN ADVANCED INTRABONY DEFECTS—RADIOGRAPHIC BONE-FILL RESOLUTION AT 1-YEAR FOLLOW-UP
Objectives: This study aimed to evaluate radiographic bone fill of advanced intrabony defects 1 year after regenerative periodontal surgery with enamel matrix derivative (EMD). Methods: Ten intrabony defects were treated with scaling root planing (SRP) + MIST + EMD. Radiographic bone-fill was were compared at baseline and after 12 months. Results: Radiographic bone fill showed an enhanced mean number of pixels (p=0.0022). Conclusion: Intrabony defects can be treated successfully by regenerative strategies with EMD as shown by comparisons at baseline and after 12 months. -


COX INHIBITORS SUPPRESS THE DIFFERENTIATION OF HUMAN OSTEOSARCOMA CELLS
Objectives: Recent reports of impaired bone healing associated with non-steroidal anti-inflammatory drugs (NSAIDs) have raised major concerns. This study was aimed to evaluate the effect of COX inhibitors in osteoblastic differentiation of osteoblast-like human osteosarcoma (HOS) cells and to evaluate whether selective COX-1 and COX-2 inhibitors have different effects on osteoblastic differentiation using HOS cells. Methods: HOS cells were cultured with selective COX-1 inhibitors (SC-560) and selective COX-2 inhibitors (NS-398). Cell numbers were counted and cell activity was measured using a WST-1 assay for 5 days of culture. Expression of alkaline phosphatase (ALP), bone morphogenetic protein (BMP)-2, bone sialoprotein (BSP) and osteocalcin (OCN) mRNA was evaluated by reverse transcriptase polymerase chain reaction (RT-PCR). Osteoblastic differentiation in cell cultures was also characterised by ALP activity. Results: SC-560 and NS-398 treatment did not inhibit cell activity below the concentration of 50nM and 1μM, respectively. Gene expression of BMP-2, BSP and OCN was not changed when HOS cells were treated with SC-560, whereas ALP mRNA expression was decreased when treated with 50nM and 100nM SC-560. ALP, BMP-2 and BSP gene expression was not changed in the HOS cells treated with NS-398, whereas OCN gene expression was prominently decreased when treated with NS-398 above concentrations of 100nM. A decrease in ALP activity after 5 days of culture was observed in SC-560- and NS-398-treated cells. Conclusions: These results suggest that COX inhibitors at higher concentrations suppress the osteoblastic differentiation of HOS cells and downregulate osteoblast-related genes. The mechanism of action of selective COX-2 inhibitors also differs from that of COX-1 inhibitors. The long-term use of high-dose NSAIDs for the control of pain and inflammation after dental surgery could have a negative effect on bone healing and on the outcome of bone management. -


BONE AUGMENTATION WITH XENOGRAFT ASSOCIATED WITH BONE MARROW ASPIRATE CONCENTRATE (BMAC)
Objectives: To evaluate bony reconstruction of atrophic anterior maxilla using particulate grafts with or without autologous BMAC obtained via the BMAC method. Methods: Patients with atrophic anterior maxillae due to tooth loss (n = 8) were selected and split into groups according to the type of material used: the control group (n=4) received particulate xenograft only, the test group (n= 4) received a combination of particulate xenograft and bone marrow aspirate concentrate obtained via the BMAC method. Both groups received a collagen membrane to cover the xenograft. After 4 months, during implant placement, a bony sample was removed from the graft area using a trephine bur with a 2-mm internal diameter. The specimens were fixed and preserved for histomorphometric assessment of the following tissues: vital mineralised tissue (VMT), non-vital mineralised tissue (NVMT) and non-mineralised tissue (NMT). Cone-beam CT (CBCT) was performed three times to measure bony thickness: (i) prior to graft insertion, (ii) 4 months after grafting, and (iii) 8 months after grafting. The parameter used was local bone gain in millimetres. Results: Tomographic analysis revealed an increase in bony tissue in the CG of 3.78+1.35mm and 4.34+1.58mm at 4 months and 8 months, respectively. The TG showed an increase of 3.79+0.52mm and 4.09+1.33mm after 4 months and 8 months, respectively. Histomorphometric analysis revealed CG values for VMT, NMT and NVMT of 11.34±5.23%, 44.45±5.5% and 40.96±12.40%, respectively, and 64.31±9.12%, 32.41±10.38% and 0.73±0.56% for the TG. Conclusions: The use of a bone marrow aspirate concentrate obtained via BMAC increased bone formation in the graft area in the anterior maxilla. -


ECTOPIC IMPLANTATION OF HYDROXYAPATITE (HA) SCAFFOLD ASSOCIATED WITH BONE MARROW ASPIRATE CONCENTRATE OR OSTEODIFFERENTIATED BONE MARROW MESENCHYMAL STEM CELLS
Objectives: To evaluate the influence of bone marrow cells on bone formation in an ectopic subcutaneous model in mice. Methods: Six BALB/c mice were divided into three groups (n = 2 in each). In all groups, a xenograft was implanted subcutaneously. In the negative control group, the xenograft was hydrated with saline solution. In the positive control group, it was embedded with osteodifferentiated adult mesenchymal stem cells derived from bone marrow. In the experimental group, the xenograft was embedded with bone marrow aspirate concentrate. After 4 weeks, the animals were sacrificed and prepared for histologic, histomorphometric and immunohistochemical analysis. The following tissues were evaluated: pre-osteoid tissue (POT), loose connective tissue (LCT) and remaining xenograft particles (XG). Results: There was statistically significant difference (p=0.008) in POT area between the negative control group (0+0%) and the other two groups (42+11% experimental; 56+55% positive control). Similarly, there was a statistically significant difference (p=0.006) in LCT area between the negative control group (49+18%) and the other two (3+9% experimental; 0+0% positive control). There were no statistically significant differences between all three groups for XG area (p=0.143). Conclusions:The use of a mineralised scaffold loaded with either concentrated bone marrow aspirate or with osteogenically-induced bone marrow mesenchymal stem cells favours the formation of osteoid tissue compared to scaffold alone. -


CLOSURE OF LARGE PERFORATIONS OF SINUS MEMBRANE USING A PEDICLED BUCCAL FAT PAD (PBFP) GRAFT
Objectives: Migration of dental implants into the maxillary sinus is an uncommon but increasing complication. Several reports demonstrate successful use of the pedicled buccal fat pad (PBFP) graft for reconstructing medium to large maxillary defects. The aim of this case study was to evaluate the outcome of a large sinus-membrane perforations closed using a PBFP graft. Methods: The PBFP graft was used for closure of large membrane perforations. Blunt dissection was performed to enter the BFP capsule, and tissue forceps were used to draw out the contents. Meticulous manipulation was required to avoid rupturing the BFP capsule. Harvested BFP was draped into the sinus and fixed to the perforated membrane using sutures, taking care not to damage the long buccal branches of the facial nerve in the facial space alongside Stenson’s duct, or the BFP itself. Results: We repaired several large sinus-membrane perforations using a PBFP graft in a single patient. Healing without complication took place within 3 weeks and the surface of the fat pad was converted to normal mucosa. Conclusions: Thorough treatment planning is critical to minimise the risk of dental implants migrating into the maxillary sinus cavity. Large membrane perforations, in which migration of implants during the insertion of healing abutment may occur, can be reconstructed immediately using a PBFP graft. The PBFP looks promising as a safe and easy method for closure of large membrane perforations. -
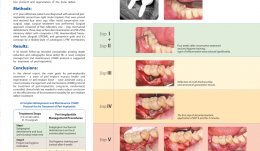

A NOVEL APPROACH FOR REGENERATIVE TREATMENT OF PERI-IMPLANTITIS: A CASE REPORT AND PROPOSAL OF A PROTOCOL
Objectives: The aim of this report was to propose guidelines for managing peri-implantitis including a three-step decontamination protocol and regeneration of a bone defect using autologous leukocyte and platelet-rich fibrin (L-PRF)-enriched composite graft, and to evaluate the radiographic defect fill and various clinical parameters. Methods: A 57-year-old woman was diagnosed with advanced peri-implantitis around two right molar implants that were placed and restored 4 years ago. Clinical examination revealed probing depth (PDs) of up to 12 mm, with bleeding and suppuration. After initial conservative non-surgical treatment, surgery was performed. The approach consisted of flap reflection, one-step mechanical debridement, three-step surface decontamination and fill of the intrabony defect with composite L-PRF, demineralised freeze-dried bone allograft (DFDBA), and gentamicin graft. Coverage was with a double-layer of autologous L-PRF membrane. Results: At 24-month follow-up there was a considerable reduction in probing depth and radiographic bone defect fill. Conclusions: The main treatment goals for peri-implantitis (peri-implant mucosa health and regeneration of peri-implant bone) were achieved using a novel complex management and maintenance (CMM) protocol for treatment of peri-implantitis. Long-term, randomised, controlled clinical trials are needed to produce robust data on the effectiveness of this treatment modality for treatment of peri-implant defects. -
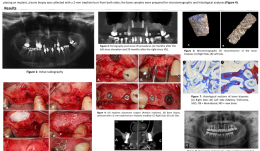

BONE FORMATION AT 12 MONTHS AND 20 MONTHS AFTER SINUS ELEVATION SURGERY WITH INORGANIC BOVINE BONE—A SPLIT-MOUTH CASE REPORT WITH MICROTOMOGRAPHIC AND HISTOLOGICAL EVALUATION
Objectives: Rehabilitation of the posterior edentulous maxilla using a dental implant is challenging when bone volume is limited. The literature supports the use of sinus lift procedures for increasing bone volume by filling the sinus cavity with autogenous bone and/or bone graft substitutes. This study reports on a patient with clinical, tomographic, microtomographic and histomorphometric evaluation of the resorption of Bio-Oss[tm] after maxillary sinus floor augmentation. Methods: A 55-year-old, non-smoking woman presented with limited bone volume on both sides of the posterior edentulous maxilla that required rehabilitation. She had no systemic problems that might affect the surgical procedures. Preoperative cone-beam CT revealed significant maxillary sinus pneumatisation. Sinus lift procedures were performed on both sides of the maxilla, using a lateral surgical approach, and the maxillary sinuses were filled with a bovine bone graft substitute (BioOss[tm] small particles). A 25x25-mm collagen membrane (BioGide[TM]) was placed over the graft and the surgical flaps were sutured to entirely cover the membranes. Postoperative medications were amoxicyillin 500mg, clavulanic acid 125mg, ibuprofen 200mg and PerioGard[TM] rinse. Sutures were removed 14 days after surgery. Healing was uneventful, with no membrane exposure or other complications. After 12 months, further cone-beam CT showed significant gains in bone volume in both maxillary sinus areas, supporting the installation of osseointegrated implants. The patient postponed implant placement surgery; the left side was reopened 12 months after sinus lifting and the right side after 20 months. Before placing an implant, a bone biopsy was collected with a 2-mm trephine bur from both sides and samples were prepared for microtomographic and histological analysis. Results: Four months after implant installation, the healing abutments were connected and cone-beam CT was performed to evaluate the implants. Provisional prostheses were then installed and remained in function for 3 months, allowing functional analysis of the prosthetic rehabilitation. Definitive ceramic crowns were then installed. Microtomography showed newly formed bone (27%) and residual biomaterial (39%). Biopsy samples at 20 months post-operatively contained [ok?] 52% newly formed bone and 16% residual biomaterial. These results revealed the process of particle resorption and replacement by new bone tissue between 12 and 20 months. Histological analysis demonstrated remnants of biomaterial particles surrounded by newly formed bone without connective tissue. There were no signs of inflammation and there was no gap between the bone and Bio-Oss[tm] particles. The biopsy collected at 20 months showed noticeably fewer particles of residual biomaterial than that collected at 12 months. Conclusion: This report showed that an inorganic bovine bone graft associated with collagen membrane can be used successfully in this sinus lift procedure for the subsequent installation of dental implants. There was slow resorption of particles and continuous replacement by newly formed bone, which are desirable for to maintaining grafted bone volume for a longer period. It is important to emphasize that this report is not intended to change the protocol for installation of implants after sinus lifting using inorganic bovine bone and collagen membrane. The extended implant placement times (12 and 20 months) described here related to the patient's situation and are not necessary or desirable in clinical practice. -
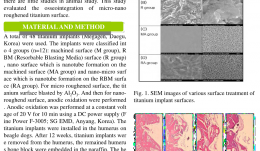

OSSEOINTEGRATION OF MICRO-NANO ROUGHENED TITANIUM SURFACES
Objectives: Anodic oxidation treatment of titanium surfaces is widely studied because of the rapid osseointegration and biocompatibility of the material, however there are few studies in animals. This study evaluated the osseointegration of micro-nano roughened titanium surface. Methods: A total of 48 titanium implants (MegagenTM/®) were used. They were classified into four groups (n=12): machined surface (group M), resorbable blasting media (RBM) surface (group R), nano surface (nanotube formation on the machined surface) (group MA), and nano-micro surface (nanotube formation on the RBM surface) (group RA). The micro-roughened surface was produced by blasting the titanium surface with aluminium oxide, and the nano-roughened surface was produced by anodic oxidation at a constant voltage of 20 V for 10 minutes with a DC power supply (Fine Power F-3005TM/®, SG EMD, Anyang, Korea). The titanium implants were placed in the humerus of beagle dogs. After 12 weeks, they were removed. Humerus bone blocks were embedded in paraffin and stained using haematoxylin–eosin. Results: Histological analysis of the bone block revealed no inflammation around implants. New bone formation was observed along the nano-micro titanium implant surfaces. After 12 weeks, lamellar bone was formed along the nano-micro titanium implant surfaces. Conclusions: Micro-nano roughened titanium implants surfaces show good osseointegration. -


MANAGEMENT OF CONGENITALLY MISSING LATERAL INCISORS WITH ORTHODONTICS AND SINGLE-TOOTH IMPLANTS
approach. Dental implants are an appropriate treatment option for replacing these teeth in adolescents when their dental and skeletal development is complete. This case report describes the orthodontic treatment of a patient with permanent dentition who had congenitally missing maxillary lateral incisors. After orthodontic treatment, the missing incisors were replaced with implants. Methods: A 21-year-old woman with congenitally missing maxillary lateral incisors was referred to our clinic. Her medical and dental history was evaluated. The treatment plan included orthodontic treatment and space opening for implant placement and correction of the occlusion. Results: The major objectives of treatment were achieved. Molar and canine class I relationships were achieved with overjet and overbite within the normal range. Panoramic radiographs showed good radicular parallelism and no signs of root resorption. Dental implants were placed in lateral incisor sites. Conclusions: Dental implants are the treatment of choice for most patients with congenitally missing lateral teeth. The preserve tooth structure and alveolar bone and provide aesthetics and function. However, successful restorative treatment involving implants depends on interdisciplinary treatment planning, especially if preprosthetic orthodontic tooth alignment is required. -


List of recommended reading
This document provides you with a list of articles/ publications recommended by the EAO Education Committee. Please note that we are working towards providing direct links to the articles which are available on COIR, this should be available in the next few weeks. In the meantime, please note that articles published in COIR can be accessed via the Student's Club or via your member area on the eao website.










