-

Study Protocols: Osseointegration Of Dental Implants
based on the book chapter by Giovanni E. Salvi, Dieter D.Bosshardt, and Niklaus P. Lang Summary The authors explain the rationale behind these techniques and how more in vivo studies of wound healing and tissue formation in humans are needed because most of the existing evidence relates to in vitro animal studies. The protocol has four phases: planning, surgery, laboratory processing and data analysis. It offers an opportunity to obtain standardized, reproducible evidence on the dynamic osseointegration process and allows comparisons to be made between implants with different designs, features and placement sites, for example, and preoperative and postoperative care regimens. It covers enrolment and selection of patients with third molar extractions and good bone volume for undergoing the split-mouth procedure, with details of the healing time points and patient care, and clear images of the procedure. The relevance of implant composition and surface properties (e.g. roughness and wettability) is explained, and the creation of a U-shaped wound compartment in the implant is described, with landmarks that can be identified after explantation. The interface that forms between the implant and bone is evaluated in terms of the bone-to-implant contact (BIC), with endpoints being determined by histology and histomorphometry to reveal immune responses and morphological changes. Microarray gene profiling is used to correlate clinical and molecular events with inflammation, angiogenesis and neurogenesis. The authors remind investigators to engage a biostatistician at an early stage. Open full-text PDF (1.3 MB) -


Study Protocols: Treatment Of Peri-Implantitis
based on the book chapter by Suzanne Mason, Feng Wang, andDarnell Kaigler Summary Treatment of peri-implantitis is a growing area of practice that would benefit from evidence gained from reproducible studies following a standardized protocol. The protocol described here allows evaluation of the effectiveness of anti-infective surgical procedures and interventions through prospective case series and randomized controlled trials. It can be used to study the nature of implantitis, bacterial plaque formation or compare different implant devices. The research question, timeline and patient care routine are specified, with advice on the baseline characteristics, bone loss thresholds and peri-implant probing. Patient eligibility criteria include defined bone loss thresholds and probing depth associated with suppuration or bleeding. The timeline covers recruitment, screening, baseline measurements and treatment, and follow-up of 12 months, with 5 years required to monitor reoccurrences. The cause-related interventions are either non-surgical, using debridement with or without antimicrobial treatment, or surgical, involving mucoperiosteal flap elevation, removal of granulation issue, defect assessment, decontamination of the implant surface and stabilization of defects using bone substitutes, grafts or bioactive substances. The postoperative antimicrobial care regimen involves maintenance care over several months. The authors emphasize the need for calibration of the force of probing and choice of instruments such as a paralleling device for standardizing radiographs. Open full-text PDF (1.3 MB) -


Study Protocols: Regeneration Of Keratinized Gingiva
based on the book chapter by Michael K. McGuire Summary There is an extensive body of evidence relating to soft tissue keratinization and the mucogingival junction (MGJ). This chapter provides an overview of the subject, and revisits the anatomy of the tooth periodontium. The protocol it describes is a randomized trial that targets patients with two non-adjacent sites of one to four tooth spans and less than 2mm of keratinized gingiva. The pre-surgical phases include screening and baseline observations, and the procedure involves comparing an apically positioned flap plus vestibuloplasty (benchmark treatment) with a new therapy. The protocol describes preferred techniques for probing and taking punch biopsies, and specifies dimensions of the wound bed. The authors recommend removing existing keratinized gingiva from the mucosal flaps so that results with the gingival graft are more discernible. They give specific instructions on the method of taking clinical photos. Post-surgical evaluations take place over 6 months, and include patient-reports of postoperative pain and discomfort at the treatment and harvest sites, with inflammatory assessment by a scoring system and measures of apicocoronal width. Other practical recommendations include the use of probes that are calibrated for studies and a 3-mm biopsy punch for revealing the MGJ, as well as allowing a learning curve for surgical techniques, possible pilot patient procedures, carrying out batch surgeries and pre-study power calculations, and consulting a biostatistician. Open full-text PDF (1.4 MB) -


Study Protocols: Root Coverage Regeneration
based on the book chapter byAnton Sculean and Sofia Aroca Summary This protocol relates to root coverage in cases of gingival recession from trauma or disease. Good results can be obtained with a coronally advanced flap technique coupled with connective tissue grafts, but harvesting the tissue is associated with negative factors. An alternative method is soft tissue grafting as used by this protocol, which compares methods and esthetic outcomes in patients with troublesome single and multiple recessions. The selection criteria are stated clearly for patients with Miller class I, II or III gingival recessions in the maxillary or mandibular arch with apicocoronal extension and a recession depth of more than 2 mm. Recruitment is on a multicenter basis, with stratification and randomization into test and control groups, and restrictions on revealing the type of intervention to the surgeons. There are photographs of test and control sites pre-, intra- and postoperatively and at 12 months. Weekly evaluations are carried out for the first month, with a total of 14 visits over the first year. Follow-up is for 35 years. Percentage root coverage is the primary endpoint, with secondary endpoints including patient-reported pain, root sensitivity, tissue thickness and long-term stability. Potential adverse events are listed together with a grading system to assess them. The authors stress the need for surgeon learning curves and calibration of examiners, techniques and equipment, blinded procedures, and engagement of a statistician. Open full-text PDF (1.4 MB) -


Study Protocols: Soft-Tissue Augmentation
based on the book chapter by Daniel S. Thoma and Ronald E. Jung Summary Soft tissue augmentation using autogenous grafts to restore keratinized tissue volume are described here. Synthetic and biological dermal substitutes, developed initially for treating burns, offer great potential as alternatives to these grafts which have certain limitations (particularly collagen-based products). Two protocols are presented, both for randomized controlled trials. The authors specify two research questions and two sets of defined eligibility criteria, study timelines with relevant clinical steps and time points for measuring clinical endpoints, protocol-specific measures and patient care regimens. Photos are provided of surgical sites before, during and after the procedures. The first study compares autogenous palate grafts (plus an apically positioned flap) with a soft tissue substitute in patients with an implant-supported prosthesis abutted by keratinized mucosa of less than 1 mm thick. Primary outcome measures include keratinized mucosal width, as determined by probing, and parameters relating to safety and effectiveness. There are phases for pre-baseline management, surgery, follow-up of 6 months, and a 5-year assessment of long-term safety, effectiveness and esthetics. The second protocol is for soft tissue volume augmentation in patients requiring volume increase in a single-tooth gap after implant placement. The positive control is a connective tissue graft, with endpoints including gain in mucosal thickness and esthetics, and a follow-up of 3 months. Open full-text PDF (1.9 MB) -


Osteology Researcher Grants: New publications from funded studies
The results of two pre-clinical studies funded by the Osteology Foundation have been published recently in the peer-reviewed journal Clinical Oral Implants Research. The two studies reveal important findings that will help to better understand the mechanisms of bone loss and soft-tissue regeneration. Supporting research into all aspects of oral tissue regeneration is a core task of the Osteology Foundation. Over recent years, the Foundation has supported a number of pre-clinical and clinical studies that have led to about 30 publications in international peer-reviewed journals. In 2014 the results from two pre-clinical studies supported by the Osteology Foundation were published in the high-ranking journal Clinical Oral Implants Research. Both studies provide important insights into basic mechanisms in bone loss and tissue regeneration. Pre-clinical rat model for studies on osteoporosis A study by Xi Ling Liu and co-workers from Hong Kong investigated the skeletal site-specific response to ovariectomy in a rat model (Liu 2014). The investigators examined changes in bone density and microcarchitecture in different bone sites and found significant differences, which is highly relevant for other studies using this animal model for osteoporosis-related studies. After 36 weeks the researchers observed that jaw bones and cranial bones in ovariectomized rats only showed a minor reduction in bone mineral density, whilst long bones, lumber vertebra and ilium in the same animals showed significant bone loss compared to the baseline. A significant deterioration of the trabecular structure was detected in the long bones and vertebra, while jaw bones remained relatively stable. Overall, femur and tibia displayed the largest bone loss. Relevant information for further studies using the model The study by Liu et al. assessed for the first time the systemic site-specific bone loss and microarchitecture changes in ovariectomized rats, a widely used animal model that mimics the estrogen-deficiency-induced bone loss, and one which is approved by the FDA for osteoporosis. The results provide valuable information for the selection of bone sites and observation times in further studies using this animal model for osteoporosis studies a topic that is becoming increasingly important, since osteoporosis, along with the aging of the population, has developed into a relevant health burden. Crosslinked and non-crosslinked collagen matrices A different topic investigated the study by Daniel S. Thoma and his co-workers from Zurich (Thoma 2014). Their study, which was also funded by a Research Grant from the Osteology Foundation, investigated in a rat model whether the crosslinking of a collagen matrix, as well as the addition of recombinant human platelet-derived growth factor-BB (rhPDGF-BB), influenced tissue integration, angiogenesis and degeneration of the collagen matrices. Four treatment modalities were tested in an ectopic model in rats and compared for the study: the cross linked matrix with and without rhPDGF-BB, and the non-cross-linked matrix with and without rhPDGF-BB. In 50 rats, the four combinations were planted in four unconnected pouches on the back of each animal. Descriptive histology and histomorphometric assessments were performed at 2, 4, 8, 16 and 24 weeks after the surgery. Angiogenesis and stability of the collagen matrices The study showed that the compact layer of the non-cross linked matrix delayed angiogenesis and connective tissue formation, while the spongeous cross-linked matrix facilitated early vascularization and also demonstrated network presence over a longer time span. No statistically significant effects of rhPDGF-BB were observed for any of the evaluated parameters. Different characteristics for different indications These results revealed that both types of matrices can be successfully incorporated into the tissue. However, the matrix composition influenced the healing patterns. The study therefore revealed important information on the use of the two different collagen matrices for different indications, since they provide different characteristics due to their different designs. These are important findings that help to evaluate the efficacy of different matrices for different indications and to understand why such differences exist. References Liu XL, Li CL, Lu WW, Cai WX, Zheng LW. Skeletal site-specific response to ovariectomy in a rat model: change in bone density and microarchitecture. Clin Oral Implants Res. 2014 Mar 5. doi: 10.1111/clr.12360. Thoma DS, Nnni N, Benic GI, Weber FE, Hmmerle CH, Jung RE. Effect of platelet-derived growth factor-BB on tissue integration of cross-linked and non-cross-linked collagen matrices in a rat ectopic model. Clin Oral Implants Res 2014 Sep 30. doi: 10.1111/clr.12496. Further information Published studies supported by Osteology Research Grants Information on Osteology Research Grants -

New president, new board members: the Osteology Foundation has voted
The Osteology Foundation has selected three new Foundation Board members: Pamela McClain, Frank Schwarz and Istvan Urban. In addition, Mariano Sanz will become the new President from June 2015 onwards. he end of May 2015 signals the end of the term of office for three present Foundation Board members: Friedrich W. Neukam (Germany), Myron Nevins (USA) and Massimo Simion (Italy). During its meeting of 27 January 2015, the Foundation Board of the Osteology Foundation therefore selected three new members to join the ranks of the Board: Pamela McClain (USA), Frank Schwarz (Germany) and Istvan Urban (Hungary). They will succeed the outgoing members in June 2015. CV Pamela McClain CV Frank Schwarz CV Istvan Urban The term of office of the current president Christoph Hmmerle (Switzerland), who has successfully led the Foundation since it was established and strongly influenced the development thereof, will also end in May 2015. Mariano Sanz (Spain), who will take over as President of the Foundation from June 2015 onwards, was chosen as his successor. Both the Foundation Board members and the President of the Osteology Foundation are selected for a period of four years and may be chosen a second time for a further four years. Voting criteria The candidates for election are nominated by the existing Foundation Board members. The vote itself takes place by means of secret ballot. In addition to professional expertise and international standing, geographical and professional equilibrium constitutes a criterion for nominations and selection. Care is taken to ensure that various countries and cultures are given just as much consideration as the various specialist areas that figure in oral regeneration, i.e. maxillofacial surgery, oral surgery, periodontology, implantology and cell biology. A balance between practice and science is also ensured. Further organisational changes From June onwards, further organisational changes will result from the new elections. The Executive Board of the Osteology Foundation will consist of the new President Mariano Sanz (Spain), William V. Giannobile (USA) as well as Christer Dahlin (Sweden) from June onwards. The Founders Representative will also continue to be represented by Paul Note (Switzerland). Further changes will concern the configurations of the three committees. They will not be definitively decided on, however, until June 2015 when the new members take up their duties during the next Foundation Board meeting. -


New Osteology Research Scholarship Programme
Research drives advances in science, and promoting research in the field of oral tissue regeneration is one of the core activities of the Osteology Foundation. That is why the Foundation is continuously expanding its activities in this field. New in 2015: the Osteology Foundation is now offering one-year Research Scholarships for young investigators to develop their career in the field of oral tissue regeneration. The aim of the Osteology Foundation is to offer scholars an outstanding environment and expertise on clinical and basic research. Osteology Scholarship Centres The scholars will work on a research project teaming up with their mentors at one of the Osteology Scholarship Centres, which are among the worlds leading research institutes in oral regeneration. The Osteology Scholarship Centres are: University of Gothenburg (Prof. Christer Dahlin) University of Michigan School of Dentistry (Prof. William Giannobile) Medical University of Vienna School of Dentistry (Prof. Reinhard Gruber) University of Zurich (Prof. Christoph Hmmerle) Amount of funding and application details The Research Scholarships consist of 35000 Swiss Francs per scholar for a twelve month stay in one of the Osteology Scholarship Centres, and are offered annually. All young investigators with an academic affiliation can apply. The Research Scholarships are awarded based on the evaluation of a motivation letter, a curriculum vitae and a recommendation letter. Financial needs are also taken into account. Deadline for the submission of applications is May 15, 2015. Applicants will be notified about acceptance by July 15, 2015. Develop your research career in oral regeneration, andapply for an Osteology Research Scholarship now! -


Collaboration: SEPA & Osteology Foundation Award
The Spanish Society of Periodontology and Osseointegration (SEPA) and the Osteology Foundation have launched a new cooperation project, aiming to promote research in regenerative therapies, and the publication of the results. Researchers are invited to submit abstracts for a special poster presentation session and subsequent discussion at the50th Annual Meeting of the SEPA, which will take place in Valencia on 12-14 May 2016. Programme The presented work should be from the field of oral regenerative therapies. Prizes will be awarded to the three best posters. The maximum number of posters for this call is 15. The posters will be presented independently of the other posters at the Annual Meeting, having their own space and jury. The winners have the unique opportunity to present also at theNational Osteology Symposium Spain,which will be held in Barcelona in February 2017. More information about this Osteology Symposium will follow soon. Summaries of the winning entries, after review by the Editorial Committee, will also be published in the journal of the society (Clinical Periodontology). For details on online submission of abstracts, format, and required information please check the following website of the SEPA (in Spanish) Premios SEPA-Osteology Foundation Deadline: 8 April 2016 -


Ridge Preservation
The alveolar ridge is the bony tissue that surrounds a fully erupted tooth. Its structure may be compromised after extraction of the tooth, but it can be preserved by use of bone substitutes, dental implants and buccal overbuilding with soft tissue grafts. Ridge preservation techniques must be developed in animals before clinical trials in patients can be conducted, and various processes, such as wound healing, can be explored that are not feasible to study in people. Dogs are most commonly used because of their similar tooth types, root structures and fast remodeling time. Several preclinical studies are described in this chapter – mostly using the dog mandible – that compare different experimental conditions, biomaterials, grafts and implants after extraction of teeth. These provide information on the timing and sequence of extraction and grafting procedures, and timepoints for assessing tissue shrinkage and resorption of alveolar bone. Other studies address osseous resorption of flaps, the lack of a periodontal ligament, buccal overbuilding, alveolar plate resorption and inflammatory reactions. Jaw casts, morphometry, histology and high-resolution imaging are used as valid endpoints relating to the alveolar process and socket walls, and the cellular content and mineralization of tissues. The protocols outlined in this chapter will contribute to the accuracy with which preclinical studies predict responses in people. -


Core & Post System Post Cementation and Core Build Up
Nölken, RobertMaterials Checklist: Dentsply Core&Post system kit. -


Operative Therapiekonzepte zur Entfernung retinierter unterer Weisheitszähne
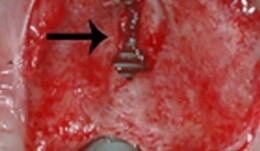
Schultze-Mosgau, Stefan / Neukam, Friedrich Wilhelm / Basting, GerdGliederung: - Schematische und röntgenologische Demonstration unterschiedlicher Retentionsformen unterer, retinierter Weisheitszähne, Darstellung der Indikation zur Entfernung - Erstellung der Behandlungsunterlagen, Aufklärungsgespräche mit Darstellung der Komplikationen - Demonstration des operativen Vorgehens: Lokalanästhesie, Schnittführung, Schutz des N. lingualis, Osteotomie, Nahttechnik. Die Entfernung unterer, retinierter Weisheitszähne gehört zu den häufigsten dento-alveolär-chirurgischen Eingriffen. Durch die enge anatomische Lagebeziehung zu den benachbarten Zähnen und dem N. alveolaris inferior besteht bei der operativen Entfernung die Gefahr einer Schädigung der umgebenden Strukturen. Die Kenntnis der verschiedenen Retentionsformen und eine geeignete, atraumatische Operationstechnik ist für eine komplikationslose Entfernung von Bedeutung. Nach der Leitungsanästhesie des N. alveolaris inferior und des N. buccalis wird die Schnittführung so gewählt, dass ein vestibulär gestielter Mukoperiostlappen gehoben werden kann. Nach dem lingualen, subperiostalen Einführen eines Raspatoriums zum Schutz des N. lingualis wird durch die bukkale Osteomie mit kugelförmigen Hartmetallfräsen der Weisheitszahn bis zu seiner größten Zirkumferenz freigelegt und durch vorsichtige Luxationsbewegungen entfernt.











