-


Immediate placement and all-ceramic restoration in the anterior maxilla - a customized interdisciplinary treatment approach
Happe, Arndt / Nolte, AndreasContents: - Patient presentation and esthetic analysis - Careful extraction of a non-salvageable tooth - Miniplast splint as a surgical template - Harvesting bone from the implant bed - Placing a CONELOG® implant at site 11 - Obtaining a corticospongeous bone cylinder at site 48 - Alveolar augmentation and reconstruction of the buccal bone lamella - Harvesting a connective-tissue graft - Tunneling the vestibular mucosa, various suturing techniques - Insertion of the provisional restorations - 3 months later: Preparing, impression and arbitrary transfer with a bite fork and facebow, temporary restoration - Master cast, new wax-up, determine the emergence profile - Fabricating a hybrid abutment, Scanning the custom abutment, on-screen crown design - Fabricating a zirconia abutment and a feldspathic ceramic veneer - Conditioning and adhesive attachment of the components, final intraoral check - Try in and adhesive cementation -


Implant-supported removable restorations in the edentulous jaw
Wolfart, Stefan / Weber, VolkerContents: - Patient presentation, impression, comprehensive jaw relation records - Wax-up, Fabrication of the provisional restoration - Fabrication of a DVT based planning and drilling template - Surgical procedures for inserting four implants in the mandible - Suturing and relining of the existing denture as a provisional restoration - After 12 weeks: Reentry and insertion of healing abutments - Harvesting a free gingiva graft to extend the attached gingiva - Verifying implant stability using Periotest - Reworking the existing denture to fit on the healing abutments - Impressioning with custom tray (pick-up technique) - Demonstrating the line finder to transfer face axis - Fabricating the three restorations with Locator® attachments, electroplated double crown, precision-milled bar - The matrix and retention parts of the Locator® system, transferring the Locator® abutments to the implants - Fabricating the electroplated copings, intraoral adhesively connecting the electroplated copings to the cast framework (passive fit), finishing and delivery - Removable restoration on a custom-milled bar, clinical and laboratory workflow, delivery - Maintaining implant-supported restorations -

Operative Therapy for Retained Teeth in the Maxilla
Schultze-Mosgau, Stefan / Neukam, Friedrich Wilhelm / Basting, GerdContent: In adolescence, the exposure and orthodontic classification of retained teeth, especially canines and premolars, represents a useful therapy measure. Techniques for surgically exposing vestibularly and palatally retained teeth are demonstrated using the tubed pedicle flap technique. Because epithelialized mucous membrane is covered in the tubed pedicle flap technique, a renewed growth of the exposed tooth is prevented and a classification of the tooth with orthodontic appliances under sight control is enabled. Depending on the retention form, the extent of movement, and the patient's age, exposure may no longer be possible under some circumstances, indicating the need for operative removal of the retained canine or premolar. Preoperative localization methods, vestibular and palatal operative access paths, and surgical techniques for atraumatic removal are demonstrated. Operative techniques for the atraumatic removal of retained maxillary third molars also are shown. For the gentle removal of retained maxillary third molars, it is very important to record their topographic positional relationship to the maxillary sinus and to select the cutting direction and most suitable osteotomy technique. Outline: - Techniques for exposing maxillary canines or premolars for orthodontic classification - Operative removal of retained maxillary canines - Operative removal of retained maxillary third molars -


Ridge augmentation in the periodontally involved dentition
Windisch, PéterContents: - Periodontal regeneration and alveolar -ridge augmentation using a connectivetissue graft - Implant insertion and augmentation - Implant re-entry and prosthetics Materials Checklist Emdogain, Bio-Oss, BioGide, Block fixating screw for autologous bone cylinder, 4/0 and 5/0 sutures, Resolut membrane Titanium pins, Autologous bone chips, 2 Replace Groovy Tapered 4, 3x13 mm implants -


Microsurgical apical resection
Nölken, Robert -


Microsurgical apical resection on a maxillary premolar
Nölken, Robert -


Esthetic and Restorative Dentistry - Dental Photography
Terry, Douglas A. -


-


THE OSTEOLOGY CASE BOX
The Osteology CASE BOX contains cases uploaded for different clinical scenarios. User decides whether they want to share their cases, or whether they only add the data for overall evaluation and compare it with the mean. -

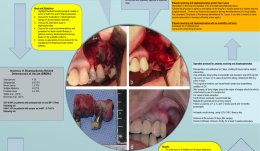
THE ROLE OF MULTIDISCIPLINARY APPROACH IN A CASE OF LANGERHANS CELL HISTIOCYTOSIS WITH INITIAL PERIODONTAL MANIFESTATIONS
Objectives: The present case epitomizes the clinical situation of a single-system Langerhans cell histiocytosis (LCH) mimicking aggressive periodontitis in a patient with no other clinical signs. Although this is a single observation, we highlight the importance of using a multidisciplinary approach in rare conditions like this for optimizing patient management. Methods: A 32-year-old Caucasian woman visited a private dental practice in Brescia, Italy, complaining of sensitivity in her mandibular left first molar. Clinical and radiographic examinations revealed recession, furcation involvement, mobility and severe alveolar bone loss, leading to a diagnosis of localised aggressive periodontitis. Over the next 3 years, the patient received non-surgical periodontal treatment, but failed attend successive follow-up appointments for undisclosed reasons. Her periodontal condition continued to worsen and multiple tooth extractions were carried out due to progressive periodontal destruction with impaired healing and development of ulcerative lesions. Panoramic radiographs were taken, and revealed severe alveolar bone destruction with “floating teeth” appearance, and an osteolytic bone lesion at the left angle of the mandible. With an overall clinical deterioration, and the possibility of an underlying malignant condition, the patient was referred for deep analysis. Results: No abnormalities were detected in laboratory and biochemical tests. Skull and sinus radiography revealed a 5-mm oval radiolucency at the left angle of the mandible. Then a radiograph of the lower leg revealed multiple osteolytic bone lesions of the left tibia. Bone-marrow aspiration and biopsy were performed to determine the nature of these lesions. Histopathology revealed a dense nodular proliferation of CD1a-positive and S100-positive Langerhans cells within bone, on a background of lymphocytic and granulocytic cells, consistent with LCH. An additional biopsy of the intra-oral lesion showed mature, disease-free, compact bone. However, a bone biopsy may be not representative of the entire structure, particularly in cases of intraoral localisation of LCH. Bidirectional Sanger sequencing analysis and pyrosequencing of DNA extracted from bone tissue of the tibia detected the presence of the BRAF-V600E hotspot somatic mutation, confirming a clonal origin of the neoplastic cells. Multidisciplinary investigations showed that the periodontal involvement was a manifestation of an underlying systemic disease (multifocal single-system LCH). The patient was then started on radiotherapy and but improvement of her oral and periodontal condition is yet to be confirmed. Conclusions: In the present case, LCH was unrecognised for several years. The periodontal disease progressed rapidly, leading to loss of most of the dentition, with persistent delays in soft tissues healing after extraction. Close monitoring of the oral signs may have allowed earlier diagnosis of LCH and prevent such rapid deterioration, possibly resulting in a better endpoint. Dentists and periodontists should be aware that rare systemic diseases such as LCH can produce oral manifestations as the first clinical sign. Such patients benefit from a multidisciplinary approach to identify and manage such entities. -

A REVIEW OF BISPHOSPHONATES—POSSIBLE MODES OF ACTION, ALTERNATIVE DRUGS AND IMPLICATIONS FOR DENTAL IMPLANT TREATMENT
Objectives: The review aimed to explore the pharmacophysiological modes of action of both oral and intravenous bisphosphonates and the potential for adverse events in patients receiving dental implant treatment. It aimed to gather evidence on the use of alternative drugs to bisphosphonates, as well as current recommendations and guidelines for dental implant therapy in patients receiving bisphosphonates. It was hoped to devise a clinical protocol for the management of bisphosphonate-treated patients. Methods: A Medline search was conducted to identify articles from the medical and dental literature between 1950 and 31 December 2014 according to well-defined inclusion and exclusion criteria. Searches were made of the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials and Embase for English-language studies published between 2000 and 31 December 2014. All cited references in the identified papers were cross-checked to ensure that no articles were missed. Given the rarity of studies with a sufficiently large prospective sample to determine the rate of failure (often over 10,000 patients are needed to achieve statistical significance), the heterogeneous studies yielded in this search (in terms of both design and outcome measures) were only suitable for descriptive analysis, rather than a meta-analysis. Results: The initial search of Medline and Embase yielded a total of 37 articles on bisphosphonates and dental implants. On further investigation, only 27 met the study inclusion criteria. There were eight retrospective studies and two case series evaluating the success rate of dental implants in patients with a history of bisphosphonate use, and another 17 articles consisting of case series and case reports. They described incidences of bisphosphonate-related osteonecrosis of the jaw in dental implant patients. In addition, two relevant articles from the Cochrane Library addressed interventions for treating osteonecrosis of the jaw bone associated with bisphosphonates. A second search of Medline and Embase for “bisphosphonates” (MeSH term) in conjunction with “oral soft tissues”, “oral hard tissues”, “avascular necrosis”, “jaw bone” and “modes/mechanisms of action” yielded a total of 51 English-language studies in humans. Late implant failures are reported in patients treated with oral bisphosphonates for more than 3 years, especially if they have existing integrated implants. Early failures are reported in patients treated with bisphosphonates before or at the time of implant placement. Most organisations agree that a safe approach is the best policy for dealing with patients on oral bisphosphonatess, by assessing the risks on an individual basis and obtaining appropriate consent. This requires close communication with the prescribing physician before surgical intervention. Several alternative drugs are available and their risks profiles also need to be determined in this context. Conclusion: Although many of the studies identified here have shortcomings, there does appear to be some risk associated with both implant placement and maintenance of osseointegrated implants in patients who take oral bisphosphonates. -












