-

Study Protocols: Osseointegration Of Dental Implants
based on the book chapter by Giovanni E. Salvi, Dieter D.Bosshardt, and Niklaus P. Lang Summary The authors explain the rationale behind these techniques and how more in vivo studies of wound healing and tissue formation in humans are needed because most of the existing evidence relates to in vitro animal studies. The protocol has four phases: planning, surgery, laboratory processing and data analysis. It offers an opportunity to obtain standardized, reproducible evidence on the dynamic osseointegration process and allows comparisons to be made between implants with different designs, features and placement sites, for example, and preoperative and postoperative care regimens. It covers enrolment and selection of patients with third molar extractions and good bone volume for undergoing the split-mouth procedure, with details of the healing time points and patient care, and clear images of the procedure. The relevance of implant composition and surface properties (e.g. roughness and wettability) is explained, and the creation of a U-shaped wound compartment in the implant is described, with landmarks that can be identified after explantation. The interface that forms between the implant and bone is evaluated in terms of the bone-to-implant contact (BIC), with endpoints being determined by histology and histomorphometry to reveal immune responses and morphological changes. Microarray gene profiling is used to correlate clinical and molecular events with inflammation, angiogenesis and neurogenesis. The authors remind investigators to engage a biostatistician at an early stage. Open full-text PDF (1.3 MB) -


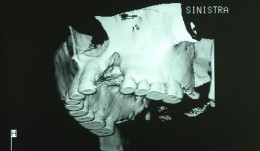
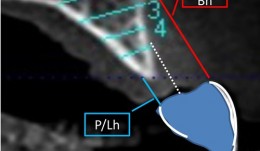
Study Protocols: Maxillary Sinus Floor Elevation
based on the book chapter by Gustavo Avila-Ortiz andPablo Galindo-Moreno Summary This technique is used to gain bone height in posterior atrophic maxillary segments before implant placement. It is increasingly used in patients with maxillary sinuses that are too close to the upper jaw or excessive bone reabsorption from gum disease. Endpoints relate to the amount of new bone formation after grafting and survival of implants and implant-supported prostheses. and long-term success rates are high. It is also excellent for studying healing following grafting with different materials and regenerative strategies in large craniofacial defects. The protocol described here is based on a hypothetical study, and covers patient screening, selection, enrolment and randomization, including a sample size calculation (which is omitted in most published studies). There are multiple phases for planning and executing the sinus elevation, followed by post-operative evaluation, and further planning and placement of implants. Detail is given on the length and form of patient visits for evaluations using cone-beam CT, impressions, photos, clinical measures, bone biopsies and adverse events recording. The discussion is supplemented by images of bone core histology and diagrams of the paranasal sinuses, and the authors point out the difference between crestal and lateral approaches. The lateral approach is illustrated throughout, including follow-up at 24 weeks and implant placement. The authors also address the problems of membrane perforation and nasal meatus occlusion. Open full-text PDF (1.9 MB) -

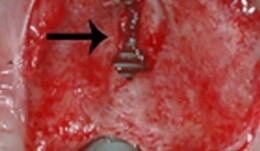
Study Protocols: Vertical Ridge Augmentation
based on the book chapter by Isabella Rocchietta, David Nisandand Massimo Simion Summary This chapter reviews the need for standardized research into vertical ridge augmentation procedures because restoring bone volume after trauma or disease is clinically challenging; the outcomes are unpredictable, the complication rates are high and success is limited. The presented protocol involves initial augmentation surgery comprising a composite graft of autogenous bone and deproteinized bovine bone, with tenting screws and a PTFE membrane overlay, followed 6 months later by surgical removal of the membrane and screws and placement of an implant. Guided bone regeneration is compared with a gold standard two-stage procedure using autogenous bone strips with deproteinized bovine particles and a titanium-reinforced membrane. The timeline incorporates a 6-month evaluation phase and further evaluation 4 months later, with a 5-year follow-up. Patient numbers and selection criteria are defined, along with suitable endpoints, care routines and the use of cone-beam CT to assess bone gain and quality. The descriptions are illustrated by CT images, radiographs and clinical photographs that show preparation of the donor and implant sites in both surgical phases. The evaluation phase relates to responses of the defect over time in terms of resorption of graft particles, soft tissue swelling, inflammation, and bone destruction and formation. What the protocol aims to do is improve outcomes for patients with traumatic tooth extractions, jaw damage, endodontic infections and failed implants. Open full-text PDF (1.4 MB) -

Study Protocols: Horizontal Ridge Augmentation
based on the book chapter by Nikos Donos and Nikos Mardas Summary This protocol focuses on measuring radiographic bone levels on the buccal side of augmented areas around implants after horizontal ridge augmentation, rather than at interproximal sites (a limitation of most published studies). The design offers a standardized means to assess graft materials, bone fillers and bone substitutes for horizontal ridge preservation, allowing comparisons of resorbable and non-resorbable materials and natural and synthetic membranes. It includes two randomized controlled trials for patients with bone defects from destructive gum disease who need local ridge augmentation before implantation. One trial uses a simultaneous technique whereby implants are placed in bone augmented with a new bone substitute plus a new or standard membrane, or a standard collagen membrane plus deproteinized bovine bone mineral; this trial comprises two phases surgical implantation and observation. The other trial is a staged technique comprising a new block-bone graft/substitute plus a new or standard membrane, and autogenous block bone graft plus a standard collagen membrane; this has a third phase. A 1-year timeline and 5-year follow-up is suggested for both trials. The authors cite various histologic and radiographic endpoints, photon bubble oscillations, peri-implant bone preservation, implant survival, patient morbidity, adverse events and patient-related outcomes. Images are provided of the change in bucco-palatal/lingual alveolar ridge width 6 months after the procedure. Open full-text PDF (1.3 MB) -


Study Protocols: Periodontal Regeneration
based on the book chapter by Pierpaolo Cortellini Summary This chapter relates to regeneration of intrabony defects, presenting a protocol that is designed to enhance clinical success rates by standardizing all aspects of the studies in this area surgical approaches, skills and training, calibration of materials and investigators, and defect morphology and patient factors. The design is for a randomized parallel group controlled trial with two treatment arms, both using combination therapy: the test group receives a modified papilla preservation technique (MPPT) plus bovine mineral material and a collagen membrane; the control group receives MPPT plus flap surgery without biomaterials. The biomaterials prevent soft tissue collapse into the defect, and the surgical flaps protect the treated area and reduce wound failure. A suitable number of patients with severe periodontitis is calculated, with recruitment advised through multiple centers. Photographs are provided of the entire surgical procedure from probing to flap closure. The timeline comprises up to 60 days pre-trial workup and 3-monthly post-surgical evaluations for a year to assess all structural and functional changes. The clinical assessments required relate to both molecular and cellular changes (e.g. plaque score, pocket depth, gingival margin and coronal papilla position) and the authors suggest methods for reporting adverse events and obtaining patient-reports, including their quality of life. The protocol recommends construction of generalized linear models as part of the data analysis. Open full-text PDF (1.5 MB) -
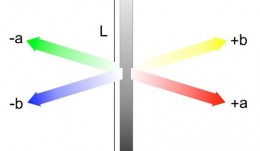

Analytical Methods: Assessment Of Esthetics And Color
based on the book chapter by Goran Benic and Irena Sailer Summary The visual appearance obtained after tissue reconstruction is an increasingly important aspect of orodental treatment, and hence of research. The esthetic aim is to achieve visual harmony between original and constructed elements. With a focus on metric assessment, the chapter offers guidance on the assessment of soft tissue levels and color matching, describing the scope and uses of ranking systems like the Copenhagen Index, Papilla Index and Implant Crown Esthetic Index, and the Pink/Pink and White Esthetic Scores. It describes how the common systems relate to different types of tissue and their optical, dimensional and surface characteristics, such as mucosal depth. While color match can be assessed using the naked eye, the growing demand for calibration and standardization makes electronic color analyzers more suitable, such as spectrophotometers, that use spectral analysis and CIE-Lab color coordinates and can be calibrated. Discussions cover all clinical parameters of interest and the factors that influence color match with the reconstruction material, such as mucosal thickness. The authors point out the need to make comparisons against healthy natural sites in the same patient, to standardize methods, minimize observer variations and ensure blind assessment. They also discuss how and when to establish baseline values to chart changes, and suggest suitable statistical analyses, with a view to publishing results the can be compared with relevant studies. Open full-text PDF (1.1 MB) -


Analytical Methods: Volumetric Measurements
based on the book chapter by David Schneider andSven Mhlemann Summary Volumetric measurements are used to detect changes in tissue dimensions in procedures such as ridge preservation and bone augmentation, and to determine tooth wear and the effects of orthodontic treatment, by converting linear dimensions into three-dimensional volumes. Both clinical and post-clinical methods are covered here. The first method comprises a single fast, simple and low-cost step that gives chairside results. Probes, endodontic files, catheters and tooth-supported stents are used to map surface topography through measures of papillary and alveolar ridge height and soft tissue thickness, among others. Reading and rounding errors may occur, however, or inconsistencies in technique, and some sites may require surgical access. Post-clinical analysis involves taking photographs, impressions, radiographs optical scans for analysis later. The authors explain how volumes are calculated from pixel or voxel counts in specified areas, and the merits of comparing approximate, absolute or relative volumes over time. Labside data can be analyzed in various ways, by different examiners, and stored for a long time. Image quality and magnification can be adjusted. Errors may occur while taking casts or processing and digitalizing data, converting file formats or superimposing datasets. The authors emphasize the need to standardize file formats, reference points, areas of interest and directions, and choose sites that are stable over time, and to calibrate all method and examiners before study startup. Open full-text PDF (1.1 MB) -


Analytical Methods: Non-Invasive
based on the book chapter by Niklaus P. Lang, Jie Han, andChristina Sim Summary Evaluations of osseointegration in the first few weeks after implant placement may reveal that biologically bonded tissue is still mechanically unstable. There is no standard procedure for assessing primary stability, but this chapter reviews progress with a non-invasive technique known as resonance frequency analysis (RFA). This is sensitive to certain aspects of the boneimplant interface and is quantified as the implant stability quotient (ISQ) which, when measured over time, indicates the extent of bone anchorage. The authors explore the relation between ISQ values and bone characteristics, bone volume density and bone trabecular connectivity, referring to controlled longitudinal clinical studies using the new Osstell mentor instrument and Straumann implants to illustrate their reproducibility and reliability, and providing a range of normative values at which healing is established in different bones in terms of homeostasis and implant stability. The authors also refer to a study that has calculated a drop in ISQ value of a specific magnitude that represents a loss of stability. The ISQ is affected by variations in morphologically different bones and the width, length and surface configuration of implants; it is not affected by implant diameter and surface modification, or instrument position. An in vitro comparison with removal torque and axial load response is also described, whereby RFA is the only method capable of detecting changes in both bone density and cortical thickness. Open full-text PDF (1.3 MB) -


Analytical Methods: Biomarkers And Molecular Biology
based on the book chapter by Alpdogan Kantarci Summary The focus of this chapter is on the range of biomarkers used currently in orodental research at both laboratory and chairside levels. With definitions of what they are, the many different types (ranging from immune factors and hormones to genetic material of disease-causing bacteria and patients) and how they relate to surrogate markers and determinants, it explains how they provide dynamic, specific and accurate measures of disease status, that can be used to supplement information gained from conventional analytical methods. However, the chapter points out their enormous potential for predicting and diagnosing disease, for profiling patient risk, identifying deviations from healthy (before clinical manifestations occur), improving clinical decision-making and facilitating personalized therapy. Drawing on studies of wound healing and regenerative therapies, the authors describe various molecular methods including immunoassays, mass spectrometry, cell cultures, PCR-based assays and newer breakthroughs such as checkerboard hybridization. They review current areas of research into costs, processing time, and normal levels in various tissues (e.g. crevicular fluid, plaque and saliva) in addition to how they vary with individual factors such as gender, ethnicity and age. In clinical trials, cross-sectional longitudinal study designs and integration of clinical and laboratory data are recommended to deal with the complexities of orodental disease. Open full-text PDF (1.2 MB) -


Study Protocols: Treatment Of Peri-Implantitis
based on the book chapter by Suzanne Mason, Feng Wang, andDarnell Kaigler Summary Treatment of peri-implantitis is a growing area of practice that would benefit from evidence gained from reproducible studies following a standardized protocol. The protocol described here allows evaluation of the effectiveness of anti-infective surgical procedures and interventions through prospective case series and randomized controlled trials. It can be used to study the nature of implantitis, bacterial plaque formation or compare different implant devices. The research question, timeline and patient care routine are specified, with advice on the baseline characteristics, bone loss thresholds and peri-implant probing. Patient eligibility criteria include defined bone loss thresholds and probing depth associated with suppuration or bleeding. The timeline covers recruitment, screening, baseline measurements and treatment, and follow-up of 12 months, with 5 years required to monitor reoccurrences. The cause-related interventions are either non-surgical, using debridement with or without antimicrobial treatment, or surgical, involving mucoperiosteal flap elevation, removal of granulation issue, defect assessment, decontamination of the implant surface and stabilization of defects using bone substitutes, grafts or bioactive substances. The postoperative antimicrobial care regimen involves maintenance care over several months. The authors emphasize the need for calibration of the force of probing and choice of instruments such as a paralleling device for standardizing radiographs. Open full-text PDF (1.3 MB) -


Study Protocols: Regeneration Of Keratinized Gingiva
based on the book chapter by Michael K. McGuire Summary There is an extensive body of evidence relating to soft tissue keratinization and the mucogingival junction (MGJ). This chapter provides an overview of the subject, and revisits the anatomy of the tooth periodontium. The protocol it describes is a randomized trial that targets patients with two non-adjacent sites of one to four tooth spans and less than 2mm of keratinized gingiva. The pre-surgical phases include screening and baseline observations, and the procedure involves comparing an apically positioned flap plus vestibuloplasty (benchmark treatment) with a new therapy. The protocol describes preferred techniques for probing and taking punch biopsies, and specifies dimensions of the wound bed. The authors recommend removing existing keratinized gingiva from the mucosal flaps so that results with the gingival graft are more discernible. They give specific instructions on the method of taking clinical photos. Post-surgical evaluations take place over 6 months, and include patient-reports of postoperative pain and discomfort at the treatment and harvest sites, with inflammatory assessment by a scoring system and measures of apicocoronal width. Other practical recommendations include the use of probes that are calibrated for studies and a 3-mm biopsy punch for revealing the MGJ, as well as allowing a learning curve for surgical techniques, possible pilot patient procedures, carrying out batch surgeries and pre-study power calculations, and consulting a biostatistician. Open full-text PDF (1.4 MB) -












