-
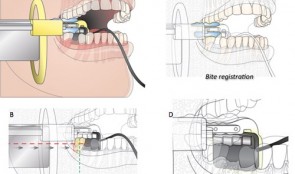

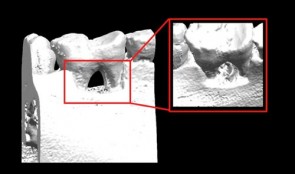
Analytical Methods: Imaging
based on the book chapter by Erika Benavides and Hector F. Rios Summary Clinical imaging allows qualitative and quantitative assessment of hard and soft oral tissues in patients after procedures such as ridge augmentation. This comprehensive guide deals with in vivo and ex vivo and intraoral and extraoral methods. It covers standardized digital intraoral radiography, cone beam (CBCT) and multislice (MSCT) computed tomography, subtraction radiography, ultrasound, optical coherence tomography (OCT), and newer methods such as CAD/CAM (computer-aided design/computer-aided manufacturing) and fractal analysis. There are descriptions on how each modality words, and outlines of their common applications, relative merits and limitations. Among the issues addressed are wave type (e.g infrared versus ionizing radiation), signal noise, distortion, mage resolution, field of view, scanning time, patient trauma and artifacts such as beam-hardening. Illustrations are used throughout to clarify the discussion. The authors point out which methods are preferable for macrostructure, and which for microstructure; for mineralized tissues, and which for soft tissue contours. Some are better for revealing the functions and dynamics of tissues or volumetric changes; some are better at 3-D visualizations and complex typography; some involve exposing patients to ionizing radiation. The authors stress the importance of integrating information from different modalities (such as CAD/CAM with CBCT) and from different time points, to optimize information available for interpretation. Open full-text PDF (1.8 MB) -
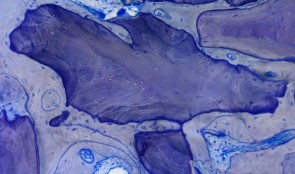

Analytical Methods: Histology
based on the book chapter by Dieter D. Bosshardt Summary Histological assessment, which can be quantitative or qualitative, is an indispensable tool for investigation of soft tissue regeneration. Harvesting tissues raises ethical considerations, but less invasive forms of evaluation, such as clinical measures and imaging, only complement the descriptive analysis, rather than replace it, by showing how cells respond to biomaterials in vivo. This chapter explores various methods for evaluating hard and soft oral tissues, such as histomorphometry, in situ hybridization and autoradiography, in the context of procedures like socket preservation, ridge augmentation and sinus floor elevation. As well as outlining suitable endpoints and landmarks, it discusses tools and techniques for taking biopsies, cutting, sectioning and embedding samples, and the use of microscopy and illumination. The authors address the challenges posed by different biomaterials -- not all can be sectioned, and some react with the chemicals used for processing samples. Thus tissue sections may be of unpredictable quality and be affected by artifacts introduced before fixation (if the tissue gets crushed during harvesting or contaminated by oral pathogens) or during fixation or preserving. Other challenges include the acquisition, processing, analysis and storage of digital images, and the huge variations in analytical equipment and methods used in different laboratories, where the need to apply laboratory standards and minimize examiner variation is emphasized. Open full-text PDF (1.9 MB) -


Statistical Analysis
based on the book chapter by Jrg Hsler Summary This chapter will enable clinical investigators to select statistical methods that extract results and conclusions from quantitative data which are both meaningful and can be compared with findings of other studies. Among the key issues discussed are the need to develop a data analysis plan, to engage a biostatistician early in the design process, and to conduct a power analysis to determine how many participants should be recruited and how many to include in treatment and control groups. There are explanations of different types of randomization processes (simple, stratified, balanced or computer-generated), error probabilities and error corrections, data distribution, and rejection of the null hypothesis on the basis of a statistical test decision. The authors explain how to choose suitable endpoints and analytical tools for specific clinical scenarios that relate to the study hypothesis. The role of descriptive measures, statistical estimates and graphs is made clear, including the concepts of confidence intervals, means, medians and standard deviations. They also describe how statistical models such as analysis of variance (ANOVA) are used to explore relations between variables, and one-way and two-way tests are used to explore relations between impact factors. The role of multiple testing is clarified, and the use of Tukey and Bonferroni corrections, Newman--Keulbs, Scehhe and Dunn devices, and Fishers least significant device (LSD) in error correction. Open full-text PDF (1.1 MB) -


Horizontal Ridge Augmentation
Ridge augmentation is sometimes needed to establish proper soft and hard tissue support before placing a dental implant. The horizontal augmentation procedure is commonly used in dental clinics to restore bone defects in people with destructive gum disease. There are many variables to investigate to optimize these treatments, for which several animal models exist. Defects can be created surgically in skeletally mature animals to study changes over time. The site of both defects and implants can also be varied, and the merits of staged or simultaneous tooth extraction and insertion of implants can be evaluated. Different types of graft material (block, particulate or autogenous), bone fillers and bone substitutes can be applied, and resorbable and non-resorbable, natural and synthetic membranes can also be compared. A major aim of these studies is to identify procedures and materials giving the most predictable outcomes. The chapter describes valid endpoints evaluated by histomorphometry, specific staining techniques, and a host of imaging modalities. It also covers other aspects of successful, reproducible experiments, such as planning, report writing, ethical approval, funding applications and submission, with the overall aim of producing new, safe clinical innovations that rapidly restore quality of life to patients. -


Ridge Preservation
The alveolar ridge is the bony tissue that surrounds a fully erupted tooth. Its structure may be compromised after extraction of the tooth, but it can be preserved by use of bone substitutes, dental implants and buccal overbuilding with soft tissue grafts. Ridge preservation techniques must be developed in animals before clinical trials in patients can be conducted, and various processes, such as wound healing, can be explored that are not feasible to study in people. Dogs are most commonly used because of their similar tooth types, root structures and fast remodeling time. Several preclinical studies are described in this chapter – mostly using the dog mandible – that compare different experimental conditions, biomaterials, grafts and implants after extraction of teeth. These provide information on the timing and sequence of extraction and grafting procedures, and timepoints for assessing tissue shrinkage and resorption of alveolar bone. Other studies address osseous resorption of flaps, the lack of a periodontal ligament, buccal overbuilding, alveolar plate resorption and inflammatory reactions. Jaw casts, morphometry, histology and high-resolution imaging are used as valid endpoints relating to the alveolar process and socket walls, and the cellular content and mineralization of tissues. The protocols outlined in this chapter will contribute to the accuracy with which preclinical studies predict responses in people. -
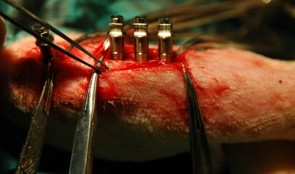

Osseointegration of Implants
The complex process of osseointegration involves formation of an interface between a dental implant and the host’s bone, without intervening soft tissue. Formation depends on qualities of the implant surface, such as its roughness and porosity, as well as characteristics of the host. Titanium coatings offer a good osseointegration surface. After preliminary tests to characterize bone-contacting materials and toxicity reactions, animal models are used to assess different aspects of bone remodeling. This chapter describes several studies for determining the biocompatibility of new implant materials, and their mechanical stability and safety. Models include the tibia of rats and rabbits, and the mandible of the dog, in which different shapes and sizes of implants and fixation techniques can be compared, and the best parameters for quantifying tissue reactions can be established. Mechanical strength testing using measures of torque and shear, for example, help determine how much bone should be in contact with the implant in order to promote osseointegration. The quality of new bone can then be assessed in terms of area, volume and extent of integration. The use of standardized methodology for sample preparation is also emphasized, with detailed description of the Donath technique, which offers many benefits but is expensive, time consuming and requires for specially trained technicians. -

Periodontal Regeneration
Animals with defects of the gum can be used to investigate the effectiveness and safety of scaffold materials, devices and biologics for bone and soft tissue repair, before they are tested in people. Living models are essential for observing changes in structure and function over time, sometimes long periods, during the remodeling and healing phases. This chapter recommends which animals are best suited for studying agents such as growth factors and barrier membranes. They include both small and large animals, such as rats, dogs and primates, with both natural defects and surgically or ligature-induced defects. The design of the studies is addressed specifically, with instructions on the creation of various standardized defects, and how to care for the animals before and after surgery, including management of biohazardous materials such as viral vectors. The roles of institutional guidelines and the requirements of regulatory bodies and animal housing authorities are also covered. Investigators who are studying the healing process sometimes need guidance on selecting suitable endpoints that can be adapted to humans in clinical settings; several measurable outcomes are specified here, based on histologic, morphometric and imaging findings, which aim to provide relevant and reproducible data on molecular and cellular responses, and entire gum tissue reactions to the intervention. -

Soft Tissue Regeneration
Stable soft tissues are essential for the stability of teeth, and patients in need of restorative therapy require a solid foundation for implants. Dental surgeons can graft healthy tissue or insert scaffold material into defective areas to promote regeneration of tissues and stimulate integration. Research has recently focused on the development of new materials that are being tested in preclinical models. Two specific methods are described in this chapter to evaluate the performance of different grafts for gain of keratinized tissue and soft tissue volume. The presented models allow studying tissue integration and regeneration and serve as standardized approaches. The rich information derived this way will make it easier to predict outcomes in humans, and hasten the use of new graft materials in patients. -


Screening Models for Tissue Engineering
These tests are carried out before preclinical studies. They are essential for exploring fundamental responses to procedures such as creating wounds in gum and bone and inserting foreign materials. Success of these interventions depends on the stability of the supporting tissues and the capacity to heal, involving the formation of blood clots and granulation tissue, and the growth of new bone and soft tissue. Screening studies tend to use small animals, often rats, to quickly and easily identify agents that show promise for preclinical studies in larger animals, which are more expensive and time consuming. The models described in this chapter include rats with induced defects of the long bones, the mandibular symphysis and ramus, and the calvarium, and addresses their suitability for testing different shapes, features and locations of implants. These studies yield information on biocompatibility at cellular, vascular and biochemical levels, as well as responses to surgical trauma and repair. The chapter emphasizes the need to use standardized, validated screening protocols to generate reproducible results, and cites specific protocols developed by various international organizations. If all screening tests meet certain basic criteria on study variables, control groups and the accessibility, homogeneity and mechanical stability of implant sites, they will comply with regulatory requirements and allow easy comparison with the existing evidence base. -


Research Design and Biostatistical Considerations
The findings of studies are of little value without proper statistical analyses that reveal the power of the results, and separate them from events that occur simply by chance. Robust analysis also allows patterns to be observed and comparisons to be made with similar studies. However, the field of statistics can be confusing and overwhelming. This chapter provides an easily understandable summary of the key principles and parameters involved, and the aims of different statistical tests. The describes real preclinical studies on bone regeneration to illustrate concepts such as variance and skew, probability, distribution, standard deviations, and categorical and non-independent data. It also gives guidance on the importance of sample size, replication and specific methods like split-mouth designs. The main focus is on an efficient top–down approach, whereby statistical analysis starts before the study begins, and sometimes involves obtaining the advice of a qualified statistician. The role of generating explicit and biologically valid questions or hypotheses is highlighted, and the need to determine adequate sample sizes and control conditions, with suitable endpoints and collection of only relevant data. Planning the analytical approach in this way produces clinically applicable results and allows meaningful conclusions to be drawn within and across studies. As such, getting the statistics right is essential for translating laboratory findings into clinical practice.











