-

Ethical Aspects In Clinical Research
based on the book chapter by Klaus Peter Rippe Summary This chapter deals with the moral and ethical minefield faced by all investigators conducting clinical experiments in patients. Obtaining histological material for studies of tissue regeneration can be ethically compromising, and any intervention may lead to burdens as well as benefits for patients, even after robust studies in animal models. In the absence of a clear concensus on morality or a simple philosophical stance, the authors focus on the principals of proportionality and equipoise, the potential for risk, international justice, and protecting patients from exploitation due to geographical or socioeconomic factors. They stress the importance of obtaining voluntarily consent from every participant, or surrogate decisions for vulnerable patients, and highlight the need for leaving no doubt about what might happen during the trial and the potential for harm. The obligation to help all patients poses unique issues: some are simply fixed, for example by comparing a new therapy with the current best one (rather than no therapy or placebo); and others are complex. However, it is acknowledged that when a particular trial arm offers more potential than one or more other arms of the study, any patient who gains a benefit also provides a means to benefit others. The doctorpatient relationship is also examined in this chapter, particularly clinicians who must recruit their own trial participants, for example when conducting preventive oral health trials among school-children. Open full-text PDF (1 MB) -


Regulatory And Good Clinical Practice Aspects In Clinical Practice
based on the book chapter by Gudrun Denke Summary It is critical for researchers conducting patient-oriented research to attend to the regulatory aspects of their studies and employ good clinical practice (GCP) throughout. This chapter provides an overview of GCP in both Europe and the USA, with valuable summaries of the many processes involved when preparing to conduct trials on medical devices, drugs and biologics in regenerative surgery, with a particular focus on the content and scope of ISO 14155:2011. The regulatory documentation is described, such as investigator brochures, case report forms, and clinical investigation plans. They authors go into detail about meeting ethical, quality and national standards through appropriate clinical investigation planning and monitoring. They draw attention to the roles and functions of sponsors and principal investigators, as well as CE marking and trial termination. The importance of assigning risk to medical devices and products is also discussed, whereby absorbable materials, bone morphogenic proteins, dental lasers and subperiosteal implants are deemed to carry significant risks, while caries-removal solutions, fillers and traditional cushions pads are considered insignificant. The four phases of trials for drugs and biologics are also outlined, together with the need for a separate classification scheme for medical devices that comprises exploratory (first-in-human), confirmatory (safety and efficacy) and post-marketing follow-up (improvement) phases. Open full-text PDF (1.1 MB) -


Peri-implantitis Defect
Inserting implants immediately after tooth extraction reduces clinic appointments, but some patients experience breakdown of their gum and bone tissues; this early exposure of the implant inhibits bone regeneration and implant success. Increasing numbers of people have implants nowadays, more of which contain titanium, which is good for osseointegration, but tends to harbor bacteria if the surrounding bone shrinks away. Preclinical research is therefore important for investigating the nature of implantitis and its relations to bacterial plaque formation. Flap procedures need to be optimized to ensure adequate wound closure and prevent wound breakdown. To this end, inflammation resembling that encountered by dentists is induced in animals by allowing plaque to accumulate or placing cotton ligatures on the gum. It is difficult to create standardized defects, but valuable observations can be made on the timings of extraction and implantation, healing periods and plaque control. The efficacy of treatments for preventing tissue loss can be assessed, as well as options for antimicrobial decontamination. Investigators can rely on the clinical relevance of the endpoints described here, which involve assessment by probing of peri-implant pockets, determining the level of the alveolar bone crest, the amount of bone–implant contact and the extent of inflammatory cell infiltrates. This remains a rich area for research in a growing area of practice. -
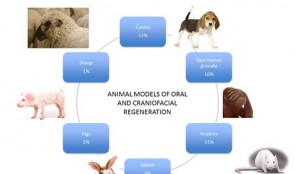

Pre-Clinical Model Development
Technological advances in engineering materials and biological agents continue to provide new potential therapies for patients whose quality of life and physical well-being are affected by severe orofacial defects, tooth loss or the consequences of gum disease. However, getting new therapies into everyday use by dental surgeons is not simple. Currently, only one in every thousand newly developed materials reaches patients, in a process that can take decades, and incurs enormous costs. To ensure that all suitable therapies developed in the laboratory become available to dentists, preclinical studies in animals must streamline neatly with clinical trials in humans, which can only happen if approval is gained by the regulatory authorities. This chapter provides guidance on the many practical issues that must be addressed before, during and after conducting animal experiments, in order to achieve the rigorous safety, efficacy and quality standards that must be met for human use. The emphasis is on effective planning and design, and choosing the most suitable animal models and techniques. The authors also outline ways to optimize and standardize experimental approaches, and set meaningful endpoints that translate directly into the clinical arena.










