-


Periodontal Preserve Therapy (Examples)
Clotten, StefanContent: - Periodontal maintenance therapy for teeth 34 and 35, including the regeneration of a bone defect using bone replacement material, collagen membrane and sutures. - Curettage for treatment of periodontal pockets. - Treatment of gingival pressure sores caused by tight-fitting orthodontic apparatus. - Incision of buccal attachment to relieve gingival pressure for elimination of gingival recession. -


Bone Spreading, Bone Condensing
Streckbein, RolandContent: Surgical flap creation and elevation; Use of drill template for exact determination of implant position; Implant site creation; Site preparation / tapping; Bone compaction; Insertion of the implants; Impression-taking; Wound closure; Later implant insertion; Dental lab work; Creating the model with laboratory implants; Shaping the bar frame; Adapting the laser welded frame to the model; Manufacturing the tooth replacement, Fitting the bar into the tooth replacement; Finishing work. -


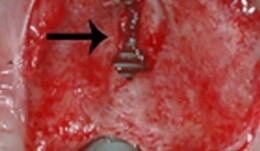
Implants for the Anterior Maxillary Region
Horrichs, Leon G.Contents: - Implant planning and positioning - Preparation - Drilling and thread-cutting - Implant insertion - Wound closure Synopsis: The implant position is determined using a drill guide/x-ray template (regions 34-32-42-44). A Peeso drill is inserted in the drill guide and used to mark the position in the mucoperiosteum. An incision is made, and the mucoperiosteum is displaced. The implant insertion sites are prepared by using a 2 mm twist drill, 2/3 mm pilot drill, 3 mm and 3/5 mm twist drills. This is followed by counter-drilling and thread-cutting. The implants were loaded at 40-50 N. The wound is then closed using GORE-TEX® suture material. -


-

THE OSTEOLOGY CASE BOX
The Osteology CASE BOX contains cases uploaded for different clinical scenarios. User decides whether they want to share their cases, or whether they only add the data for overall evaluation and compare it with the mean. -


AAP Collaboration: Workshop Proceedings published
Enhancing Periodontal Health Through Regenerative Procedures Fifty-two workshop participants met in Chicago last summer to conduct a systematic review of existing literature, culminating in the development of consensus reports and practical applications to aid practitioners in the clinical environment. Topics of the workshop included the following: Periodontal Soft Tissue Root Coverage Procedures: Managing gingival recession based on current evidence with a primary outcome goal of complete root coverage Periodontal Soft Tissue Non-Root Coverage Procedures: Assessing the need for gingival augmentation procedures (non-root coverage) around natural teeth Intrabony Defects: Periodontal regenerative strategies for the management of intrabony periodontal defects Furcation Defects: How periodontal furcation defects should be managed via periodontal regenerative therapy and what parameters should be used for treatment selection Emerging Regenerative Approaches for Periodontal Reconstruction: Can emerging technologies for periodontal regeneration become clinical reality? Each practical applications paper describes a specific clinical situation, different approaches that may be considered in its management, and how an expert makes a treatment decision based on the provided evidence. Clinical Advances in Periodontics also offers illustrative images and videos that further detail the clinical situation, how it was managed, and its expected treatment outcomes. How the workshop came to be and what the findings mean for periodontal practice The2014 AAP Regeneration Workshopon the topic Enhancing Periodontal Health Through Regenerative Procedures was of huge interest to the Osteology Foundation, and therefore it was supported with an educational grant. The international consensus meetingwas co-chaired by theOsteology BoardmembersWilliam V. GiannobileandPamela K. McClain. We are excited to announce that the proceedings of this workshop have now been published in a special supplement of the Journal of Periodontology, and are available online with free access. Proceedings of the 2014 AAP Regeneration Workshop The publication is a great result of the first joined efforts of the AAP and the Osteology Foundation. The results havedemonstrated that regenerative procedures are effective and predictable treatment options for helping patients retain their natural dentition. The workshop was an amazing collaborative effort that provides the most current consensus of therapies and technologies in regenerative treatment, sayd AAP president Joan Otomo-Corgel at a press-conference in Chicago, when the publication was announced. Were thrilled to share the results of the these dynamic discussions. This bell weather information will provide tremendous benefit to the periodontal specialty, the dental community, and the patients we treat. -


Study Protocols: Soft-Tissue Augmentation
based on the book chapter by Daniel S. Thoma and Ronald E. Jung Summary Soft tissue augmentation using autogenous grafts to restore keratinized tissue volume are described here. Synthetic and biological dermal substitutes, developed initially for treating burns, offer great potential as alternatives to these grafts which have certain limitations (particularly collagen-based products). Two protocols are presented, both for randomized controlled trials. The authors specify two research questions and two sets of defined eligibility criteria, study timelines with relevant clinical steps and time points for measuring clinical endpoints, protocol-specific measures and patient care regimens. Photos are provided of surgical sites before, during and after the procedures. The first study compares autogenous palate grafts (plus an apically positioned flap) with a soft tissue substitute in patients with an implant-supported prosthesis abutted by keratinized mucosa of less than 1 mm thick. Primary outcome measures include keratinized mucosal width, as determined by probing, and parameters relating to safety and effectiveness. There are phases for pre-baseline management, surgery, follow-up of 6 months, and a 5-year assessment of long-term safety, effectiveness and esthetics. The second protocol is for soft tissue volume augmentation in patients requiring volume increase in a single-tooth gap after implant placement. The positive control is a connective tissue graft, with endpoints including gain in mucosal thickness and esthetics, and a follow-up of 3 months. Open full-text PDF (1.9 MB) -


Study Protocols: Root Coverage Regeneration
based on the book chapter byAnton Sculean and Sofia Aroca Summary This protocol relates to root coverage in cases of gingival recession from trauma or disease. Good results can be obtained with a coronally advanced flap technique coupled with connective tissue grafts, but harvesting the tissue is associated with negative factors. An alternative method is soft tissue grafting as used by this protocol, which compares methods and esthetic outcomes in patients with troublesome single and multiple recessions. The selection criteria are stated clearly for patients with Miller class I, II or III gingival recessions in the maxillary or mandibular arch with apicocoronal extension and a recession depth of more than 2 mm. Recruitment is on a multicenter basis, with stratification and randomization into test and control groups, and restrictions on revealing the type of intervention to the surgeons. There are photographs of test and control sites pre-, intra- and postoperatively and at 12 months. Weekly evaluations are carried out for the first month, with a total of 14 visits over the first year. Follow-up is for 35 years. Percentage root coverage is the primary endpoint, with secondary endpoints including patient-reported pain, root sensitivity, tissue thickness and long-term stability. Potential adverse events are listed together with a grading system to assess them. The authors stress the need for surgeon learning curves and calibration of examiners, techniques and equipment, blinded procedures, and engagement of a statistician. Open full-text PDF (1.4 MB) -


Study Protocols: Regeneration Of Keratinized Gingiva
based on the book chapter by Michael K. McGuire Summary There is an extensive body of evidence relating to soft tissue keratinization and the mucogingival junction (MGJ). This chapter provides an overview of the subject, and revisits the anatomy of the tooth periodontium. The protocol it describes is a randomized trial that targets patients with two non-adjacent sites of one to four tooth spans and less than 2mm of keratinized gingiva. The pre-surgical phases include screening and baseline observations, and the procedure involves comparing an apically positioned flap plus vestibuloplasty (benchmark treatment) with a new therapy. The protocol describes preferred techniques for probing and taking punch biopsies, and specifies dimensions of the wound bed. The authors recommend removing existing keratinized gingiva from the mucosal flaps so that results with the gingival graft are more discernible. They give specific instructions on the method of taking clinical photos. Post-surgical evaluations take place over 6 months, and include patient-reports of postoperative pain and discomfort at the treatment and harvest sites, with inflammatory assessment by a scoring system and measures of apicocoronal width. Other practical recommendations include the use of probes that are calibrated for studies and a 3-mm biopsy punch for revealing the MGJ, as well as allowing a learning curve for surgical techniques, possible pilot patient procedures, carrying out batch surgeries and pre-study power calculations, and consulting a biostatistician. Open full-text PDF (1.4 MB) -


Study Protocols: Treatment Of Peri-Implantitis
based on the book chapter by Suzanne Mason, Feng Wang, andDarnell Kaigler Summary Treatment of peri-implantitis is a growing area of practice that would benefit from evidence gained from reproducible studies following a standardized protocol. The protocol described here allows evaluation of the effectiveness of anti-infective surgical procedures and interventions through prospective case series and randomized controlled trials. It can be used to study the nature of implantitis, bacterial plaque formation or compare different implant devices. The research question, timeline and patient care routine are specified, with advice on the baseline characteristics, bone loss thresholds and peri-implant probing. Patient eligibility criteria include defined bone loss thresholds and probing depth associated with suppuration or bleeding. The timeline covers recruitment, screening, baseline measurements and treatment, and follow-up of 12 months, with 5 years required to monitor reoccurrences. The cause-related interventions are either non-surgical, using debridement with or without antimicrobial treatment, or surgical, involving mucoperiosteal flap elevation, removal of granulation issue, defect assessment, decontamination of the implant surface and stabilization of defects using bone substitutes, grafts or bioactive substances. The postoperative antimicrobial care regimen involves maintenance care over several months. The authors emphasize the need for calibration of the force of probing and choice of instruments such as a paralleling device for standardizing radiographs. Open full-text PDF (1.3 MB) -

Study Protocols: Osseointegration Of Dental Implants
based on the book chapter by Giovanni E. Salvi, Dieter D.Bosshardt, and Niklaus P. Lang Summary The authors explain the rationale behind these techniques and how more in vivo studies of wound healing and tissue formation in humans are needed because most of the existing evidence relates to in vitro animal studies. The protocol has four phases: planning, surgery, laboratory processing and data analysis. It offers an opportunity to obtain standardized, reproducible evidence on the dynamic osseointegration process and allows comparisons to be made between implants with different designs, features and placement sites, for example, and preoperative and postoperative care regimens. It covers enrolment and selection of patients with third molar extractions and good bone volume for undergoing the split-mouth procedure, with details of the healing time points and patient care, and clear images of the procedure. The relevance of implant composition and surface properties (e.g. roughness and wettability) is explained, and the creation of a U-shaped wound compartment in the implant is described, with landmarks that can be identified after explantation. The interface that forms between the implant and bone is evaluated in terms of the bone-to-implant contact (BIC), with endpoints being determined by histology and histomorphometry to reveal immune responses and morphological changes. Microarray gene profiling is used to correlate clinical and molecular events with inflammation, angiogenesis and neurogenesis. The authors remind investigators to engage a biostatistician at an early stage. Open full-text PDF (1.3 MB) -


Study Protocols: Maxillary Sinus Floor Elevation
based on the book chapter by Gustavo Avila-Ortiz andPablo Galindo-Moreno Summary This technique is used to gain bone height in posterior atrophic maxillary segments before implant placement. It is increasingly used in patients with maxillary sinuses that are too close to the upper jaw or excessive bone reabsorption from gum disease. Endpoints relate to the amount of new bone formation after grafting and survival of implants and implant-supported prostheses. and long-term success rates are high. It is also excellent for studying healing following grafting with different materials and regenerative strategies in large craniofacial defects. The protocol described here is based on a hypothetical study, and covers patient screening, selection, enrolment and randomization, including a sample size calculation (which is omitted in most published studies). There are multiple phases for planning and executing the sinus elevation, followed by post-operative evaluation, and further planning and placement of implants. Detail is given on the length and form of patient visits for evaluations using cone-beam CT, impressions, photos, clinical measures, bone biopsies and adverse events recording. The discussion is supplemented by images of bone core histology and diagrams of the paranasal sinuses, and the authors point out the difference between crestal and lateral approaches. The lateral approach is illustrated throughout, including follow-up at 24 weeks and implant placement. The authors also address the problems of membrane perforation and nasal meatus occlusion. Open full-text PDF (1.9 MB)










