-


Treatment of a fenestration defect with GBR and CT graft
João Batista Cesar Neto -


-


-


Patient forms
Patient Consent for Sedation: Required to be filled out by YOU and signed by your patient before patient takes any sedation medication. Submitted to the Education Coordinator, Andrew, prior to surgery, along with the main Consent Form. If no sedation, the main Patient Consent form needs to be filled out and submitted to Andrew prior to surgery. Patient Care is a double-sided one-page handout that you can give to your patients. This handout contains both a map location for the UBC clinic as well as basic directions and guidelines for your patient to be aware of. -

-

-

-

-

-
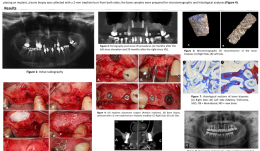

BONE FORMATION AT 12 MONTHS AND 20 MONTHS AFTER SINUS ELEVATION SURGERY WITH INORGANIC BOVINE BONE—A SPLIT-MOUTH CASE REPORT WITH MICROTOMOGRAPHIC AND HISTOLOGICAL EVALUATION
Objectives: Rehabilitation of the posterior edentulous maxilla using a dental implant is challenging when bone volume is limited. The literature supports the use of sinus lift procedures for increasing bone volume by filling the sinus cavity with autogenous bone and/or bone graft substitutes. This study reports on a patient with clinical, tomographic, microtomographic and histomorphometric evaluation of the resorption of Bio-Oss[tm] after maxillary sinus floor augmentation. Methods: A 55-year-old, non-smoking woman presented with limited bone volume on both sides of the posterior edentulous maxilla that required rehabilitation. She had no systemic problems that might affect the surgical procedures. Preoperative cone-beam CT revealed significant maxillary sinus pneumatisation. Sinus lift procedures were performed on both sides of the maxilla, using a lateral surgical approach, and the maxillary sinuses were filled with a bovine bone graft substitute (BioOss[tm] small particles). A 25x25-mm collagen membrane (BioGide[TM]) was placed over the graft and the surgical flaps were sutured to entirely cover the membranes. Postoperative medications were amoxicyillin 500mg, clavulanic acid 125mg, ibuprofen 200mg and PerioGard[TM] rinse. Sutures were removed 14 days after surgery. Healing was uneventful, with no membrane exposure or other complications. After 12 months, further cone-beam CT showed significant gains in bone volume in both maxillary sinus areas, supporting the installation of osseointegrated implants. The patient postponed implant placement surgery; the left side was reopened 12 months after sinus lifting and the right side after 20 months. Before placing an implant, a bone biopsy was collected with a 2-mm trephine bur from both sides and samples were prepared for microtomographic and histological analysis. Results: Four months after implant installation, the healing abutments were connected and cone-beam CT was performed to evaluate the implants. Provisional prostheses were then installed and remained in function for 3 months, allowing functional analysis of the prosthetic rehabilitation. Definitive ceramic crowns were then installed. Microtomography showed newly formed bone (27%) and residual biomaterial (39%). Biopsy samples at 20 months post-operatively contained [ok?] 52% newly formed bone and 16% residual biomaterial. These results revealed the process of particle resorption and replacement by new bone tissue between 12 and 20 months. Histological analysis demonstrated remnants of biomaterial particles surrounded by newly formed bone without connective tissue. There were no signs of inflammation and there was no gap between the bone and Bio-Oss[tm] particles. The biopsy collected at 20 months showed noticeably fewer particles of residual biomaterial than that collected at 12 months. Conclusion: This report showed that an inorganic bovine bone graft associated with collagen membrane can be used successfully in this sinus lift procedure for the subsequent installation of dental implants. There was slow resorption of particles and continuous replacement by newly formed bone, which are desirable for to maintaining grafted bone volume for a longer period. It is important to emphasize that this report is not intended to change the protocol for installation of implants after sinus lifting using inorganic bovine bone and collagen membrane. The extended implant placement times (12 and 20 months) described here related to the patient's situation and are not necessary or desirable in clinical practice. -
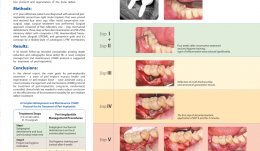

A NOVEL APPROACH FOR REGENERATIVE TREATMENT OF PERI-IMPLANTITIS: A CASE REPORT AND PROPOSAL OF A PROTOCOL
Objectives: The aim of this report was to propose guidelines for managing peri-implantitis including a three-step decontamination protocol and regeneration of a bone defect using autologous leukocyte and platelet-rich fibrin (L-PRF)-enriched composite graft, and to evaluate the radiographic defect fill and various clinical parameters. Methods: A 57-year-old woman was diagnosed with advanced peri-implantitis around two right molar implants that were placed and restored 4 years ago. Clinical examination revealed probing depth (PDs) of up to 12 mm, with bleeding and suppuration. After initial conservative non-surgical treatment, surgery was performed. The approach consisted of flap reflection, one-step mechanical debridement, three-step surface decontamination and fill of the intrabony defect with composite L-PRF, demineralised freeze-dried bone allograft (DFDBA), and gentamicin graft. Coverage was with a double-layer of autologous L-PRF membrane. Results: At 24-month follow-up there was a considerable reduction in probing depth and radiographic bone defect fill. Conclusions: The main treatment goals for peri-implantitis (peri-implant mucosa health and regeneration of peri-implant bone) were achieved using a novel complex management and maintenance (CMM) protocol for treatment of peri-implantitis. Long-term, randomised, controlled clinical trials are needed to produce robust data on the effectiveness of this treatment modality for treatment of peri-implant defects. -


CLOSURE OF LARGE PERFORATIONS OF SINUS MEMBRANE USING A PEDICLED BUCCAL FAT PAD (PBFP) GRAFT
Objectives: Migration of dental implants into the maxillary sinus is an uncommon but increasing complication. Several reports demonstrate successful use of the pedicled buccal fat pad (PBFP) graft for reconstructing medium to large maxillary defects. The aim of this case study was to evaluate the outcome of a large sinus-membrane perforations closed using a PBFP graft. Methods: The PBFP graft was used for closure of large membrane perforations. Blunt dissection was performed to enter the BFP capsule, and tissue forceps were used to draw out the contents. Meticulous manipulation was required to avoid rupturing the BFP capsule. Harvested BFP was draped into the sinus and fixed to the perforated membrane using sutures, taking care not to damage the long buccal branches of the facial nerve in the facial space alongside Stenson’s duct, or the BFP itself. Results: We repaired several large sinus-membrane perforations using a PBFP graft in a single patient. Healing without complication took place within 3 weeks and the surface of the fat pad was converted to normal mucosa. Conclusions: Thorough treatment planning is critical to minimise the risk of dental implants migrating into the maxillary sinus cavity. Large membrane perforations, in which migration of implants during the insertion of healing abutment may occur, can be reconstructed immediately using a PBFP graft. The PBFP looks promising as a safe and easy method for closure of large membrane perforations.















