Objectives:
The present case epitomizes the clinical situation of a single-system Langerhans cell histiocytosis (LCH) mimicking aggressive periodontitis in a patient with no other clinical signs. Although this is a single observation, we highlight the importance of using a multidisciplinary approach in rare conditions like this for optimizing patient management.
Methods:
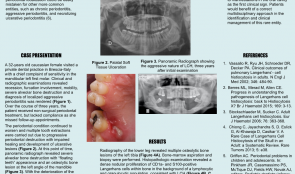
A 32-year-old Caucasian woman visited a private dental practice in Brescia, Italy, complaining of sensitivity in her mandibular left first molar. Clinical and radiographic examinations revealed recession, furcation involvement, mobility and severe alveolar bone loss, leading to a diagnosis of localised aggressive periodontitis. Over the next 3 years, the patient received non-surgical periodontal treatment, but failed attend successive follow-up appointments for undisclosed reasons. Her periodontal condition continued to worsen and multiple tooth extractions were carried out due to progressive periodontal destruction with impaired healing and development of ulcerative lesions. Panoramic radiographs were taken, and revealed severe alveolar bone destruction with “floating teeth” appearance, and an osteolytic bone lesion at the left angle of the mandible. With an overall clinical deterioration, and the possibility of an underlying malignant condition, the patient was referred for deep analysis.
Results:
No abnormalities were detected in laboratory and biochemical tests. Skull and sinus radiography revealed a 5-mm oval radiolucency at the left angle of the mandible. Then a radiograph of the lower leg revealed multiple osteolytic bone lesions of the left tibia. Bone-marrow aspiration and biopsy were performed to determine the nature of these lesions.
Histopathology revealed a dense nodular proliferation of CD1a-positive and S100-positive Langerhans cells within bone, on a background of lymphocytic and granulocytic cells, consistent with LCH. An additional biopsy of the intra-oral lesion showed mature, disease-free, compact bone. However, a bone biopsy may be not representative of the entire structure, particularly in cases of intraoral localisation of LCH. Bidirectional Sanger sequencing analysis and pyrosequencing of DNA extracted from bone tissue of the tibia detected the presence of the BRAF-V600E hotspot somatic mutation, confirming a clonal origin of the neoplastic cells. Multidisciplinary investigations showed that the periodontal involvement was a manifestation of an underlying systemic disease (multifocal single-system LCH). The patient was then started on radiotherapy and but improvement of her oral and periodontal condition is yet to be confirmed.
Conclusions:
In the present case, LCH was unrecognised for several years. The periodontal disease progressed rapidly, leading to loss of most of the dentition, with persistent delays in soft tissues healing after extraction. Close monitoring of the oral signs may have allowed earlier diagnosis of LCH and prevent such rapid deterioration, possibly resulting in a better endpoint. Dentists and periodontists should be aware that rare systemic diseases such as LCH can produce oral manifestations as the first clinical sign. Such patients benefit from a multidisciplinary approach to identify and manage such entities.