-


DENTAL IMPLANT SURVIVAL IN HYPODONTIA PATIENTS: A RETROSPECTIVE STUDY
Objectives: Specialists in prosthodontics and restorative dentistry are often challenged by oral rehabilitation of patients with hypodontia. Implant rehabilitation is commonly used to replace developmentally missing teeth, but evidence of implant survival in hypodontia patients is scarce. The aim of this study was to present findings on short- to medium-term clinical outcomes, complications and survival rates of dental implants in patients with hypodontia who were treated in Birmingham, UK. Methods: A retrospective analysis was conducted of the clinical records of patients treated within the Oral and Maxillofacial Surgery Department at Queen Elizabeth Hospital and the Restorative Dentistry Department at the University of Birmingham Dental Hospital. All patients were identified from the hypodontia clinic database. Clinical variables were recorded, collated and compared with reports of adverse events during a follow-up period of up to 6.7 years. Patient data were collected using a pro forma regarding the number and the location of implants, the surgical procedure, and any surgical or restorative complications. All patients on the study had a review appointment within the previous 3 months. The data were analysed to determine the number of patients treated, the type and number of implants placed, the site of placement and type of augmentation used, and to identify any peri-operative and post-operative complications. The minimum, maximum and mean follow-up period was calculated and the number of implants per follow-up year were recorded. Results: There were 67 patients aged between 20 and 57 (average 28 years) who received 304 implants to replace anterior (54.9%) and posterior (45.1%) missing tooth units; 49% of implants were placed in the maxilla and 51% in the mandible; 36.5% were placed in non-grafted sites and 63.5% in grafted sites. Mandibular ramus augmentation was used in 80.3% of cases, iliac crest augmentation in 11.9%, and bovine origin xenografts in 7.8%. Post-surgical complications were experienced by 19.4% of patients; four had fenestration or dehiscence type defects around the implant, the graft failed in two, and seven had transient anaesthesia or paraesthesia in the inferior dental nerve distribution area. There were complications in 3.2% implants after completion of the restorative treatment, 40% of which were soft tissue complications (e.g. gingival inflammation); 60% were prosthodontic complications (e.g. screw loosening or ceramic fracture). All were minor and were resolved in-office or by replacement of the prosthesis. One implant failed within the first year, producing a survival rate of 9% within the observation period of up to 6.7 years (range 0.1 to 6.7; mean 2.7 years). Reviews were carried out in 0–2 years for 39.4% of implants, in 3–5 years for 57.6%, and in 6–7 years for 3%. Conclusions: The implant survival rate was 99.6% up to 6.7 years after surgery. This is higher than the implant survival rate reported in the another published study of implants in hypodontia patients, and higher than those reported in non-hypodontia patient studies. A post-implant complication rate of 19.4% in this study is similar to that of other studies, and similar restorative complications have been found in other studies in non-hypodontia patients. Implant rehabilitation is a successful option for replacing developmentally missing teeth, but short implants should be considered in cases requiring vertical ridge augmentation, because our failure and complication rates were higher in these cases. -


STEM CELL BONE ALLOGRAFTS IN MAXILLARY SINUS AND RIDGE AUGMENTATION – REPORT OF A CASE
Objectives: To evaluate the use of an allograft cellular matrix containing live stem cells for maxillary sinus and ridge augmentations. Methods: Maxillary sinus and ridge augmentations were performed using an allograft cellular matrix containing live stem cells. The post-operative results were evaluated by CT scans and peri-apical radiographs. Sinus augmentation was evaluated after 10 weeks. Radiographic bone tomography was similar to that of the native bone and the ridge augmentation resulted in a vertical ridge augmentation of 3–4mm. The cellular matrix was supplied by Brockton, MA and processed by AlloSource, Centennial, CO. Results: Following healing and approximately 10 weeks following surgery, an additional CT scan was taken. This showed that the native and augmented bone was of an adequate width for supporting an implant. Radiography revealed that the augmented bone had a similar texture to native bone, indicating formation of mature bone. The scan also revealed downward growth of the bone in a vertical direction, overlapping the crest of the native pre-maxillary bone. This was not attempted during the surgical procedure, and was a particular cause for concern. Conclusions: This use of allograft mesenchymal stem cells has been shown to be a reliable method for ridge augmentation, especially in the vertical direction in areas of severe ridge atrophy. Further studies are needed to support this finding in a more guided manner, especially for vertical ridge augmentation. -

REAL-TIME NAVIGATION: THE BEGINNING OF A NEW ERA IN GUIDED IMPLANT SURGERY
Objectives: To demonstrate that dynamic guided surgery is as predictable as conventional surgery. Methods: Partially edentulous patients requiring a fixed rehabilitation were selected for this pilot study. No specific contraindications were established, and smokers were not excluded. An impression was taken pre-operatively using an irreversible hydrocolloid (Cavex CA37®) to fabricate a diagnostic cast for moulding the surgical stent (NaviStent®). Afterwards, a standard cone-beam CT (CBCT) scan was made with the NaviStent® in place using a Planmeca Promax 3-D Max®. Images were converted into DICOM files and transformed into a 3-D virtual model using the Navident® software. The potential implant locations were planned in a prosthesis-driven way. For preparing the osteotomy, the drilling axis of the handpiece and the twist drills were calibrated. The osteotomies were prepared at low speed using a high level of cooling. The navigation software guided the drilling procedure in real time. Before installing implants, an extra calibration procedure was performed for tracking the implant. The aim of this pilot study was to determine the clinical outcome up to 12 months post-operatively for implants installed using the Navident® guided surgery system. Results: Partially edentulous men (n = 6) and women (n = 7) were included in this pilot study (mean age 52.15 years; range 20–75). Out of these 13 patients, two were current smokers of more than 10 cigarettes per day. Twenty implants were inserted. No mechanical or biological complications occurred during the surgical procedure, and no major complaints were reported, such as hemorrhage, sinus pathology or severe post-operative pain. No implants were lost up to 1 year after insertion, resulting in 100% implant survival. Conclusions: Based on the results of this pilot study, real-time navigation is a promising technique. However, there is not yet enough evidence to show that the method is as safe and predictable as conventional implant surgery. -


ALVEOLAR RIDGE PRESERVATION IN DAMAGED SITE 4.7—AN EARLY STAGED OPEN-HEALING PROTOCOL IN HIGH-RISK PATIENTS TREATED WITH ORAL BISPHOSPHONATES
Objectives: The objective was to simplify the regenerative procedure using a minimally invasive technique. Ridge preservation at the time of the patient’s tooth avulsion was not possible because of acute infection. Surgery was performed using biomaterials during the early post-extractive healing process. The "early build-up technique", as used in healthy patients, was chosen to reduce comorbidity risks in a single high-risk patient. Methods: A 69-year-old woman had been treated with oral alendronate 70 mg weekly since 2001 because of a vertebral fracture caused by osteoporosis. She had experienced in anamnesis breast neoplasm in 2000 (and recurrence in 2015) and myocardial infarction for which she had a triple bypass in 2007 and angioplasty in 2014. The patient attended the clinic for chronic periodontitis and the tooth 4.7 was extracted because of recurrent periodontal abscesses. Before the extraction, cone beam computed tomography (CBCT) allowed evaluation of cortical wall thickness around the mobile mesial inclined 4.7 from the most significant eight cross sections (CS), and 16-mm mesiodistal bone assessment. The edentulous area 4.6 was partially included in the evaluation. Photographs were taken and periodontal probing performed 2 months after extraction of 4.7. The surgical protocol involved flapless avulsion of the tooth in October 2011 and the flap procedure 2 months later (December 2011). The early alveolar build-up was performed using bovine-derived xenograft and collagen matrix. The surgical design was restricted to keratinised gingiva 4.6–4.7. The intra-alveolar connective tissue of the thick vestibular flap was preserved and rotated on the second layer of the matrix to protect the wound. The exposed surface of the matrix resembled geometrically a post-extract alveolus and flap suture was performed without periosteal-releasing incisions to guide soft tissue proliferation (GGP; guided gingival proliferation). Results: No complications were reported after surgery. The exposed matrix surface was part of the GGP procedure. As in healthy patients, the exposed biomaterial surface was sealed after 4 weeks. The gain in keratinised gingiva was 2mm. The hard tissue outcome was detected by 16-mm mesiodistal CBCT changes before the extraction and after surgery. Before the extraction, the bone crest width in the distal area 4.7 was 6 mm in two cross-sections and 8–9 mm in three mesial cross sections (area missing 4.6). Near the roots in 4.7 in three central cross-sections, there was only 1 mm of lingual cortical wall with fenestration defects (1 CS) and vestibular bone was largely absent (>50%). The alveolar cavity was partially retentive. After lateral ridge regeneration the bone crest width was 10–12 mm in seven cross-sections, with the greatest linear horizontal bone gain (of 10 mm) in four central cross-sections. The lingual osseous fenestration was healed. Overall the lingual bone plate height in distal area 4.7 was decreased by 1–2 mm (three distal cross-sections), with no differences in central and mesial areas (five sections). The vestibular cortical wall height was 2–5 mm greater in the central and distal area 4.7 (six cross-sections), with no differences in the mesial area (two cross-sections). The vertical distance between bone crest and alveolar nerve level was 8–9 mm in all cross sections, without residual defect area. After 4 years of follow-up the 4.7 site is in a stable condition according to ortopantomography and photographs. Conclusions: In healthy patients, this surgical augmentation of horizontal alveolar bone and keratinised gingiva is problem-free, and was shown to be the case also in this high-risk patient, in whom implant surgery is contraindicated because of comorbid conditions and uncontrolled periodontitis. In healthy patients, implant insertion is possible 6–12 months after bone augmentation. The choice of the GGP protocol for this alendronate-treated patient was associated with fewer risks than surgery with primary intention healing of the wound. Further clinical trials should be conducted on the GGP protocol, and may show that covering bone substitutes with collagen matrix exposed during the early post-extractive wound healing process is a surgical step instead of a complication of the GBR procedure. -
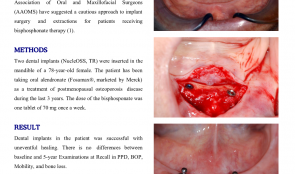

Clinical and radiografic evaluation with 5 years follow-up of two dental implant-supported mandibular overdentures in the patient receiving oral bisphosphonate therapy
Objectives: Systemic diseases may affect oral tissues by increasing their susceptibility to other diseases or by interfering with healing. Oral bisphosphonates (BP) are commonly prescribed for patients with osteoporosis to arrest bone loss and preserve bone density. The American Association of Oral and Maxillofacial Surgeons (AAOMS) have suggested a cautious approach to implant surgery and extractions for patients receiving bisphosphonate therapy. Methods: Two dental implants (NucleOSS, TR) were inserted in the mandible of a 78-year-old female. The patient has been taking oral alendronate (Fosamax®, marketed by Merck) as a treatment of postmenopausal osteoporosis disease, during the last 3 years. The dose of the bisphosphonate was one tablet of 70 mg once a week. Results: Dental implants in the patient was successful with uneventful healing. There is was no differences between baseline and 5-year Examinations at Recall in PPD, BOP, Mobility, and bone loss. Conclusion: History of oral BP use is not an absolute contraindication for dental implant placement and dental implants can be osseointegrated successfully in this patient population. Great attention should be paid to the regular dental recall for implant-prosthetic restorations. -
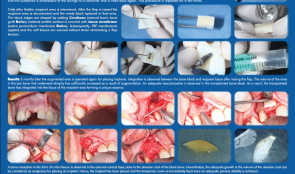

ACHIEVING A MORE EFFICIENT CONTACT SURFACE BETWEEN A BLOCK BONE AND RECIPIENT AREA USING A 3D STEREOLITHOGRAPHY (SLA) MODEL OF A JAW FRAGMENT IN ADJUSTING A HUMAN BONE BLOCK TO THE RESIPIENT AREA AND TIME SAVING DURING OPERATION
Objectives: Autogenic and allogenic bone block materials of different companies are increasingly used in guided bone regeneration (GBR) procedures. Adjusting block-shaped allogenic transplants to fit the recipient area is time consuming and technically challenging. A method of bone block formation using a 3-D stereolithography (SLA) model is reported here. Methods: A tomographic image of the area for augmentation was obtained and edited using Implant Assistant. Data from the image of the prepared 3-D jaw model were transferred to a 3-D printer (Objet Stratasys to produce a model of the jaw fragment. Unicortical cancellous block (Maxgrapht cortico-spongiosa) was moulded onto the model and holes for fixation screws were drilled into the material. The bone block was added to a 100-grams syringe filled with serum, emptied out in to a container and refilled. This procedure was repeated several times. After raising a flap, the recipient area was decorticated and the prepared block put in place. The edges were shaped by adding natural bovine bone graft (Cerobone) material and the surface was covered with native pericardium membrane (Jason membrane). A platelet-rich fibrin (PRF) membrane was then applied and the soft tissues sutured without strain to avoid flap tension. Results: After 6 months, the augmented area was re-operated for implant placement. Integration was observed between the bone block and recipient tissue after raising the flap. The volume of jaw atrophied bone had increased as a result of augmentation. There was adequate vascularisation of the transplanted bone block, which was integrated into the tissue of the recipient area. Bone resorption in the form of a thin fissure was observed in the external cortical layer, close to the alveolar crest of the block. Nevertheless, the growth in alveolar crest volume was deemed adequate for implant placement. A temporary crown was fixed immediately after placement because there was adequate stability, and alveolar crest defect was re-grafted with Cerabone and covered with Jason membrane before the flap was closed. After 4 months, an image was taken that showed bone augmentation and osseointegration around the implant. Conclusions: Preparing a jaw bone fragment as an allogenic bone block using an SLA model done successfully in GBR-type surgeries. The method allows block bone to be adapted for the recipient area, and is associated with significant time savings. Post-operative tomographic scans confirm augmentation of the alveolar ridge, making this a promising way for restoring aesthetics in the frontal area. -


MANAGEMENT OF CONGENITALLY MISSING LATERAL INCISORS WITH ORTHODONTICS AND SINGLE-TOOTH IMPLANTS
approach. Dental implants are an appropriate treatment option for replacing these teeth in adolescents when their dental and skeletal development is complete. This case report describes the orthodontic treatment of a patient with permanent dentition who had congenitally missing maxillary lateral incisors. After orthodontic treatment, the missing incisors were replaced with implants. Methods: A 21-year-old woman with congenitally missing maxillary lateral incisors was referred to our clinic. Her medical and dental history was evaluated. The treatment plan included orthodontic treatment and space opening for implant placement and correction of the occlusion. Results: The major objectives of treatment were achieved. Molar and canine class I relationships were achieved with overjet and overbite within the normal range. Panoramic radiographs showed good radicular parallelism and no signs of root resorption. Dental implants were placed in lateral incisor sites. Conclusions: Dental implants are the treatment of choice for most patients with congenitally missing lateral teeth. The preserve tooth structure and alveolar bone and provide aesthetics and function. However, successful restorative treatment involving implants depends on interdisciplinary treatment planning, especially if preprosthetic orthodontic tooth alignment is required. -

-

-














