-


Complete rehabilitation of a cleft patient
Dr. Thomas HitzThe current restoration is insufficient and the supporting implants show periimplantitis. A new full-mouth rehabilitation has to be planned. This comprehensive case was treated by Dr. Thomas Hitz, Frauenfeld, Switzerland. -


Biologic Complications - Peri-implantitis
Prof. Andrea MombelliPeri-implantitis is a highly relevant topic for every dentist and surgeon placing or restoring implants. In this module, the controversy about the actual prevalence of peri-implant infections, the correct diagnosis and the right treatment approach are discussed in detail, based on the available scientific evidence. -


Laser decontamination at sites 11 and 12
Schwarz, FrankOutline: - Presentation of clinical findings - Explanations Er:YAG laser/fibre tip/power settings - Treatment - Postoperative management List of materials: Er:YAG laser device (KEY 3®, KaVo, Biberach, Germany) Laser handpiece (2061, KaVo, Biberach, Germany) Cone-shaped glass fibre tip Safety goggles Periodontal probe (PCP12, Hu-Friedy Co., Chicago, Illinois, USA) -


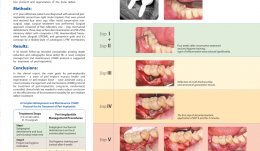
Study Protocols: Treatment Of Peri-Implantitis
based on the book chapter by Suzanne Mason, Feng Wang, andDarnell Kaigler Summary Treatment of peri-implantitis is a growing area of practice that would benefit from evidence gained from reproducible studies following a standardized protocol. The protocol described here allows evaluation of the effectiveness of anti-infective surgical procedures and interventions through prospective case series and randomized controlled trials. It can be used to study the nature of implantitis, bacterial plaque formation or compare different implant devices. The research question, timeline and patient care routine are specified, with advice on the baseline characteristics, bone loss thresholds and peri-implant probing. Patient eligibility criteria include defined bone loss thresholds and probing depth associated with suppuration or bleeding. The timeline covers recruitment, screening, baseline measurements and treatment, and follow-up of 12 months, with 5 years required to monitor reoccurrences. The cause-related interventions are either non-surgical, using debridement with or without antimicrobial treatment, or surgical, involving mucoperiosteal flap elevation, removal of granulation issue, defect assessment, decontamination of the implant surface and stabilization of defects using bone substitutes, grafts or bioactive substances. The postoperative antimicrobial care regimen involves maintenance care over several months. The authors emphasize the need for calibration of the force of probing and choice of instruments such as a paralleling device for standardizing radiographs. Open full-text PDF (1.3 MB) -

A NOVEL APPROACH FOR REGENERATIVE TREATMENT OF PERI-IMPLANTITIS: A CASE REPORT AND PROPOSAL OF A PROTOCOL
Objectives: The aim of this report was to propose guidelines for managing peri-implantitis including a three-step decontamination protocol and regeneration of a bone defect using autologous leukocyte and platelet-rich fibrin (L-PRF)-enriched composite graft, and to evaluate the radiographic defect fill and various clinical parameters. Methods: A 57-year-old woman was diagnosed with advanced peri-implantitis around two right molar implants that were placed and restored 4 years ago. Clinical examination revealed probing depth (PDs) of up to 12 mm, with bleeding and suppuration. After initial conservative non-surgical treatment, surgery was performed. The approach consisted of flap reflection, one-step mechanical debridement, three-step surface decontamination and fill of the intrabony defect with composite L-PRF, demineralised freeze-dried bone allograft (DFDBA), and gentamicin graft. Coverage was with a double-layer of autologous L-PRF membrane. Results: At 24-month follow-up there was a considerable reduction in probing depth and radiographic bone defect fill. Conclusions: The main treatment goals for peri-implantitis (peri-implant mucosa health and regeneration of peri-implant bone) were achieved using a novel complex management and maintenance (CMM) protocol for treatment of peri-implantitis. Long-term, randomised, controlled clinical trials are needed to produce robust data on the effectiveness of this treatment modality for treatment of peri-implant defects. -

-













