-
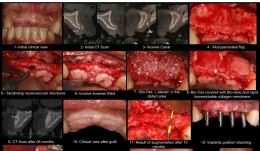

RIDGE AUGMENTATION BY APPLYING DEPROTEINISED BOVINE BONE MINERAL (DBBM) AND BIORESORBABLE MEMBRANE—A CASE REPORT
Objectives: Lateral ridge augmentations are traditionally performed using autogenous bone grafts, bone screws and titanium-reinforced ePTFE membrane; they are associated with considerable patient morbidity and a requirement for large flaps at second-stage surgery. The aim of this study was to determine whether the use of resorbable membranes and bone substitutes could lead to successful horizontal ridge augmentation, allowing the installation of implants in normal conditions, and thus minimising risks and morbidity to the patient. Methods: The patient presented with an anterior maxilla bone deficiency (canine–canine) preventing the placement of dental implants. The residual bone average was 2.5mm before bone augmentation surgery. Soft tissue flaps were carefully raised and particles of deproteinised bovine bone mineral (DBBM) (Bio-Oss[tm]) were placed in the defect area. A collagenous membrane (Bio-Gide[tm]) was applied to cover the DBBM and immobilised to the surrounding bone using only the soft tissue. The flaps were sutured to allow for healing by primary intention and to stabilise the DBBM and membrane. Results: Ten months after primary surgery, the average bone gain was 5mm and the bone crest was approximately 7mm after augmentation, allowing implant placement. When the flaps were raised for re-entry, the regenerated tissue appeared as mineralised bone tissue. Integration of deproteinised bovine bone particles into the newly formed bone was observed. Conclusion: Despite its limitations, this clinical case demonstrated that the combination of DBBM and collagen membrane may be used successfully for horizontal ridge augmentation. -


RETROSPECTIVE STUDY OF 147 IMPLANTS INSERTED IN AUGMENTED MAXILLARY SINUS AND 15-YEAR FOLLOW-UP OF MAXILLARY SINUS AUGMENTATION USING INORGANIC BOVINE BONE
Objectives: The study aimed to evaluate bone formation following maxillary sinus augmentation using bovine bone substitute material Bio-Oss[tm] and to determine the long-term success rate, using radiographic images of implants installed after sinus lifting procedure. Methods: Between January 2000 and October 2015, a total of 147 implants were placed in 64patients (24 men and 40 women), aged 34–87 years (meaan 57.39 years), in whom sinus lifting technique was performed on edentulous ridge bone (with 1–4mm residual bone height). Long-term evaluation involved comparing radiographic images at various time points from 99 cases of sinus floor elevation in the 64 patients, according to the technique described by Tatum (1986). Dental implants were inserted after 8 months of graft healing, and left submerged for 3 months. They were then loaded with provisional acrylic prostheses, which were replaced by definitive fixed metal–ceramic prostheses and followed for over 5 years of functional loading. All patients visited the clinic at 1 week, 2 months and 8 months in the first postoperative year, then at 1 year, 2 years, 5 years, 10 years and 15 years[ok?] thereafter, for clinical and radiographic examinations of the sinuses and implants, including CT imaging. Results: Twelve of the 147 implants were lost, giving a cumulative survival rate (CSR) of 91.83%. All lost implants were substituted and all patients who were followed had fixed prostheses functioning after 5 years of loading. Conclusion: This study suggests that the installation of implants after a sinus lift procedure combined with deproteinised bovine bone substitute material (Bio-Oss[tm]) graft in cases with pneumatisation of the posterior maxilla have predictable high survival rates. The procedure is a reliable option for the placement of implant-supported prostheses in patients with increased pneumatisation of the maxillary sinus and atrophic alveolar bone. -


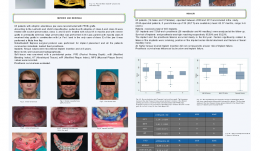
MORPHOLOGICAL EVALUATION OF SOFT TISSUE AUGMENTATION USING POROUS POLY-D, L-LACTIC ACID WITH STRAIGHT HOLES
Objectives: This study aimed to investigate the biological reaction to porous poly-d, l-lactic acid (PDLLA) scaffolds with holes for soft tissue augmentation. Methods: The control group consisted of porous PDLLA with a diameter of 5.0mm and a height of 2.0mm. For the two test groups, seven holes were drilled in the topof the scaffolds, with a diameter of 0.5mm and height 1.0mm. Each scaffold was placed in the periosteum of cranium and their height and molecular weight was measured at 4 and 8 weeks. Frozen sections were prepared from one sample from each group, to allow observation of the relationship between the material and cells. Paraffin-embedded sections were stained with haematoxylin and eosin to measure the areas of connective tissue and blood vessels. Results: The scaffolds from all groups had similar heights at 4 and 8 weeks, but their molecular weights decreased significantly over time. Significant differences were observed in connective tissue and blood vessel areas among the control scaffold no holes, and scaffolds with 0.5-mm and 1.0-mm diameter hole at both time points. Direct connection was observed between the material and cells. Conclusion: The amount of soft tissue increased with PDLLA drilled with straight holes. The straight holes kept the area of connective tissue. Neither molecular weight nor height of the scaffold were affected by the existence or size of the holes, but the area of connective tissue and blood vessels increased significantly in PDLLA containing holes, whereby holes of larger diameter showed greater areas. -
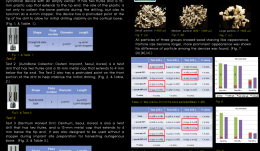

VOLUMETRIC COMPARISON OF THREE DIFFERENT INNOVATIVE BONE-COLLECTING DEVICES FOR AUTOGENOUS BONE GRAFTS
Objectives: The aim of this study was to clinically evaluate three different bone-collecting devices throughvolumetric analysis. Methods: Bone particles were harvested from bovine mandibles using three different collecting devices (1, 2 and 3) and ten drilling sites in each group. Bone particles were then filtered through sieves with openings of 500μm and 1000μm and divided into three groups according to size: 1000μm (large; LP). Total wet volume, fractional wet volume, fractional dry volume and weight were recorded and the shapes of the dried particles were examined using a microscope. Results: The bone particles in all three groups had the appearance of wood shavings. Collecting devices 1 and 2 primarily yielded LPs (0.510±0.064 mL, 0.430±0.067 mL, respectively). For device 3, MPs were most common (0.112±0.019 mL). The wet volume of both SPs and MPs obtained using device 3 was significantly greater than from devices 1 and 2 (p Conclusion: The three innovative bone collecting devices studied here collected comparable amounts of bone particles for potential use in commercial bone graft materials. -


BEHAVIOR AND DIFFERENTIATION OF OSTEOBLASTS ON A TITANIUM SURFACE WITH DIFFERENT MICROMETRE-SCALE ROUGHNESS
Objectives: Titanium implants with mean arithmetic roughnesses (Ra) of 1–2µm are associated with improved osseointegration and clinical outcome. However, the procedures used for producing a roughened surface usually change other parameters, such as spatial characteristic skewness and kurtosis, and sub-micrometre and nanoscale roughness. Studies are needed to explore the effect of different surface characteristics on osseointegration and clarify the relationship between Ra and osseointegration. This study aimed to investigate how titanium surfaces with different micrometer-scale roughnesses influenced proliferation, migration and differentiation of osteoblasts in vitro. Methods: Titanium replicas with surface roughnesses (Ra) of approximately 0µm, 1µm, 2µm and 4µm were produced. The surfaces have no significant sub-micrometre or nanoscale roughness and have similar skewness and kurtosis. MG-63 osteoblasts were cultured on the surfaces for up to 5 days and their behavior was investigated using time-lapse microscopy. The speed of cell migration was quantified using specialised software. Gene and protein expression were determined for alkaline phosphatase (ALP), osteocalcin and vascular-endothelial growth factor (VEGF). Results: Cell migration speeds were significantly lower on surfaces with Ra of about 4µm compared to those with lower Ra levels, with no differences between those with Ra in the range 0–2µm. Cell proliferation decreased gradually with increasing Ra. Gene expression of ALP, osteocalcin and VEGF was greater for the 1-µm and 2-µm Ra surfaces than the 0-µm and 4-µm surfaces. These findings were similar for protein expression. ALP and osteocalcin content in the conditioned media were significantly higher for cells grown on the 2-µm Ra surface compared to the 0-µm and 4-µm surfaces. The production of VEGF by cells on the 1-µm and 2-µm surfaces was significantly higher than that of the 0-µm surface. Cells grown on the 2-µm surface produced significantly more VEGF than those on the 4-µm surface. Conclusion: Surfaces with lower and higher roughnesses in this study seem to be suboptimal for osteoblasts. We suggest that decreased cell migration on surfaces with Ra 4µm might be associated with decreased osteoblast differentiation, probably through inhibition of cell-to-cell contact. -


EFFECT OF VITAMIN D-LOADED BONE SUBSTITUTES ON OSTEBLASTOGENESIS AND OSTEOCLASTOGENESIS IN VITRO
Objectives: Vitamin D deficiency is common, especially in elderly people, but elevating systemic levels through supplementation before surgery requires extensive effort. Local application of vitaminD-loaded bone substitutes is one alternative. However, the optimum carrier material is unknown. We assessed the effect of vitamin 25(OH)2 D3 and 1,25(OH)2 D3 (vitamin 25D, 1,25D)-loaded deproteinised bovine bone mineral (DBBM) on its own or with collagen (DBBM/C) on the genesis of osteblasts and osteoclasts. Methods: DBBM and DBBM/C were loaded with vitamin 25D and 1,25D and lyophilised. Surface structure loaded and unloaded materials was assessed using scanning electron microscopy (SEM). Release kinetics were assessed using supernatants generated after 1, 3, 6, 24 and 48 hours, and the effect of the supernatants on osteoblastogenesis and osteoclastogenesis was evaluated. MC3T3-E1-based alkaline phosphatase (ALP) was used for osteoblastogenesis; for osteoclastogenesis, RAW 264.7 cells were used in the presence of receptor activator of NF-κB ligand (RANKL) based on the numbers of multinuclear tartrate-resistant acid phosphatase (TRAP)-positive cells. MTT tests were also used to assess viability of MC3T3-E1 and RAW 264.7 cells. Results: The SEM images show no changes in the surface structure of loaded bone substitutes after loading with vitamin 25D and 1,25D. The osteoblastogenesis assays showed that supernatants of DBBM/C reduced ALP levels for up to 6 hours regardless of the type of vitamin D, while no substantial effects were observed with supernatants of DBBM alone. These findings paralleled the reduction in formazan formation in the presence of supernatants from DBBM/C taken in the first 6 hours. The osteoclastogenesis assays revealed a strong reduction in the number of TRAP-positive multinucleated cells in RAW 264.7 cultures when treated with supernatants of DBBM/C, while no substantial effects of supernatants of DBBM were observed. Overall the reduction in osteoclastogenesis was more pronounced than the reduction in osteoblastogenesis. Conclusion: Our findings suggest that regardless of the type of vitamin D used, DBBM/C has a stronger paracrine-like activity than DBBM, leading to a reduction of osteoblastogenesis and osteoclastogenesis. Overall, the inhibition of osteoclastogenesis was more pronounced, suggesting an antiresorptive effect, thus it is important to consider these properties when using bone substitute materials as carriers for vitamin D. -


IMMEDIATE LOADING IN POST-EXTRACTION SITES WITH MACHINE SURFACE IMPLANTS—A REPORT OF 63 CASES
Objectives:A recent, significant breakthrough in oral implantology was immediate implantation following tooth extraction, which reduces the number of surgical procedures required. The aim of this study was to test whether or not machine-surfaced implants, used for immediate loading of single-implant crowns in post-extraction sites, yields different results from conventional submerged two-stage implant positioning in healed sites with rough implants, in terms of implant survival after 6 months. Methods: Patients over 18 years of age requiring a single immediate post-extraction implant in the aesthetic area were enrolled in the study. The two adjacent teeth were required to be present. After gentle tooth extraction, a machine-surfaced implant (iMAXpro[TM]) with internal hexagonal connection was used. Different implant lengths and diameters were selected depending on the patient’s anatomy. Each implant was immediately loaded with a screw-retained provisional restoration. Implant insertion torque was also assessed with a manual wrench and reported as > 35 N/cm. The extraction socket had at least three intact walls, with partial dehiscence allowable on the fourth wall. If there was a residual gap of > 1mm between the implant surface and the buccal bone wall, it was filled with bone substitute (BioOss[tm] deproteinised bovine bone granules). After 6 months of follow-up, final prosthetic restoration was performed. Results: A total of 63 immediate loading post-extraction implants were positioned. All implants had uneventful healing, but five failed within 6 months. The implant success rate at 6 months was 92%. According to a defined standard, 58 implants fulfilled all the criteria of implant success: absence of persistent subjective complaints, such as pain, foreign body sensation, and/or dysaesthesia; absence of a recurrent peri-implant infection with bleeding and/or suppuration; absence of mobility; and absence of continuous radiolucency around the implant. No patients needed any additional surgical or pharmacological therapy. No implants showed signs of damage, such as fracture or bending. In 55 cases, the gap between the implant surface and buccal bone wall was > 1mm and was filled with BioOss[tm] granules, and in all cases there was a wound healing without complication, comparable to cases with no graft. Conclusion: Immediate implant placement with immediate loading provides good treatment outcomes and allows good functional and aesthetic results. It also addresses the psychosocial aspects of dental extraction. However, to achieve satisfactory results it is necessary to carefully select clinical cases and strictly apply the surgical and prosthetic protocols, with a well-trained team capable of controlling the surgical and prosthetic problems that can arise. In this study, the machine-surfaced fixture was shown to be effective for immediate loading of post-extraction implants, but it is necessary to follow-up all implants for a longer period. All patients will be checked again at 1, 2, 3, 4 and 5 years after implantation, using intraoral radiographs and aesthetic evaluation to confirm whether outcomes are comparable with conventional two-stage surgical techniques and other implant surfaces. -


PERIODONTAL REGENERATION VIA CELL HOMING
Objectives: The innate healing potential of periodontium has emerged as a new focus for regenerative therapies. Consequently, cell homing is appealing because it relies on attraction of the patient’s own stem cells. Stromal cell-derived factor-1 alpha (SDF-1α) plays a major role in this process. The aim of this study was to develop a construct for periodontal regeneration based on cell homing with SDF-1α, and to evaluate its effect on early and late wound healing in a periodontal defect model. Methods: For the preparation of the construct, gelatin sponge loaded with recombinant human SDF-1α was used. The release kinetics of SDF-1α were studied in vitro. A transwell migration model was used to test the in vitro homing capability of the SDF-1α construct for rat bone marrow stromal cells (BMSCs). Subsequently, constructs were tested for efficacy in a validated rat periodontal model. In 48 athymic nude rats, intrabony periodontal defects were created unilaterally and implanted with either (i) SDF-1α-loaded gelatin sponge, (ii) gelatin sponge, or (iii) left empty as a control for evaluation periods of 1 and 6 weeks (n=8). Evaluation consisted of descriptive histology, histomorphometry (epithelial downgrowth, inflammation, functional ligament length, new bone area, new bone height) and micro-CT (volume newly formed bone). In vivo recruitment of rat BMSCs to the defect site was tested immunohistochemically, whereby green fluorescent protein (GFP)-transgenic rat BMSCs were injected into the tail vein of the rats. GFP-positive cells in the defect site were quantified in situ by flow cytometry in 12 nude athymic rats using the same experimental set-up. All measurements were subjected to statistical analysis with ANOVA and differences were considered significant at p Results: The in vitro release experiment showed limited release of SDF-1α (picogram quantities following nanogram loading). The transwell migration model proved the site-homing capability of the SDF-1α construct in vitro for the rat BMSCs. At 1 week post-implantation, the histological tissue response in the defect was similar for all groups, with epithelial downgrowth, inflammation (30%), minor bone formation and no periodontal ligament formation. At 6 weeks post-implantation, SDF-1α constructs showed more newly formed bone area and height (0.4mm versus 0.2mm and 0.13mm versus 0.8mm), longer relative functional ligament (0.3mm versus 0.2mm) and less inflammation (6% versus 12%) compared to gelatin controls. However, the differences between the SDF-1α group and empty defects were not significant, except for newly formed bone height (14% versus 7%). Epithelial downgrowth was comparable for all groups at 1 and 6 weeks. The micro-CT data supported the histomorphometrical findings. The volume of the newly formed bone for SDF-1α constructs was significantly higher than for both gelatin and empty controls after 6 weeks (18% versus 10% and 8%). At 1 and 6 weeks post-implantation, no GFP-positive BMSCs were detected in the defect. Conclusion: The SDF-1α construct significantly improved periodontal wound healing at 6 weeks in terms of bone regeneration. In view of suboptimal release kinetics of SDF-1α from the gelatin sponge, alternative carriers need to be explored to maximise the potential for bone regenerative procedures via cell homing. -


BIOMIMETIC APPROACH TO STIMULATE OSTEOGENESIS ON TITANIUM IMPLANT SURFACES USING FIBRONECTIN-DERIVED OLIGOPEPTIDE
Objectives: Our previous studies demonstrated that a recombinant fibronectin (FN)-derived oligopeptide (F20) stimulated adhesion, proliferation and differentiation of osteoblast in vitro and in vivo. This study aimed to investigate the osteogenic potential of titanium discs coated with F20 for stimulating osseointegration on the surface of dental implants . Methods: The surface characteristics of titanium were assessed using confocal laser scanning microscopy (CLSM). Synthetic F20 was coated onto the titanium discs (machined or SLA) by an adsorption procedure. ST2 cells were then seeded onto the discs, and their adhesion was evaluated using scanning electron microscopy (SEM) and CLSM. Cell proliferation was assessed with PicoGreen staining, and osteoblast differentiation was observed using with real-time polymerase chain reaction (PCR), assessment of alkaline phosphotase (ALP) activity, immunoblot assay and ALP staining. Results: Fluorescence analysis of the fluorescein isothiocyanate (FITC)-labeled F20 disc coating showed good adsorption of F20 and different coating patterns depending on the roughness of the surface. SEM and CLSM showed that the cells were well attached to the machined surface, with greater formation of stress fibres on discs coated with F20 than on uncoated discs. The F20 coating stimulated cellular proliferation, as well as osteoblast differentiation (probably through the extracellular signal-regulated kinase (Erk) signaling pathway). Responses to F20 were slightly better with discs with a machined titanium surface than those with an SLA surface. Conclusion: These results suggest that F20 promotes osteogenesis through the Erk pathway and is a suitable biomolecule for surface modification of dental implants with the purpose of improving osseointegration. -

NOBELGUIDE IMPLANT SURGERY AND IMMEDIATE FUNCTION IN FFHB-GRAFTED PATIENTS – A RETROSPECTIVE COHORT STUDY WITH 4–6 YEARS FOLLOW-UP
Objectives: The purpose of this retrospective study was to assess the value of computer-aided technology (NobelGuideä/®) for rehabilitation of fresh-frozen homologous bone (FFHB)-grafted patients with an implant-supported, fixed full-arch prostheses. All patients were treated with a flapless surgical procedure and immediate-function protocol. Implant survival was evaluated after 4–6 years. Methods: Sixty-five patients with atrophic edentulous jaws were reconstructed with FFHB grafts. A NobelGuideä/® flapless surgical protocol was performed for implant placement and all patients received an immediate loaded fixed prosthesis. Implant torque values were recorded at insertion (T1) and after 5 years (T2). Bone levels were assessed radiographically. Soft tissue was examined with a periodontal probe. Pocket probing depth (PPD), modified bleeding index (mBI), keratinised tissue (KT), modified plaque index (mPI) and mucosal plaque scores (MPS) were recorded. Prostheses survival was evaluated. Results: Fourteen men and 51 women were operated on between 2009 and 2011. Of these, 59 (91.7%) were available at a mean follow-up of 62.37 months (range 4–6 years). There were a total of 345 implants (252 Speedy Groovyä/®, 85 MKIIIä/®. Analysis of 321 implants and 72 full-arch prostheses (26 mandibular and 46 maxillary) was performed at follow-up. Survival of implants and prostheses was high at 95.09% and 93.23%, respectively. Most implant and prosthesis failures occurred in the first year. Factors that related significantly to implant failure were smoking, position of the implant at the last distal abutment, and basal maxillary bone fracture. Prosthesis survival was influenced by bruxism and implant failure. Conclusions: This retrospective study demonstrates that computer-guided implant placement in FFHB-grafted patients is a predictable treatment modality that allows clinicians to achieve good primary implant stability, resulting in high survival rates. -


SUPPLEMENTATION OF BIO-GIDE WITH THE SECRETOME OF PLATELETS, ORAL CELLS AND HYPOXIA-MIMETIC AGENTS—EVALUATION OF RELEASE KINETICS AND BIOLOGICAL ACTIVITY IN VITRO
Objectives: Collagen barrier membranes are clinically applied in guided bone regeneration and can be loaded with bioactive factors. We investigated a novel strategy using these membranes as carriers for the secretome of activated platelets (PSEC), oral cells (OSEC) and hypoxia-mimetic agents (HMA). Methods: We measured the release of PSEC, OSEC and HMA from the collagen barrier membrane Bio-Gide. The mitogenic and pro-angiogenic effects were assessed in bioassays with human oral cells. Growth factor release was investigated by immunoassay of the supernatants taken from Bio-Gide. The release of HMA was assessed by photometry. Results: Bio-Gide releases PSEC, OSEC and HMA with a burst-like release kinetic. The release of total protein and growth factors such as platelet-derived growth factor (PDGF-BB(, transforming growth factor(TGF)-β, and vascular endothelial growth factor (VEGF) peaked in the first hours and rapidly decreased thereafter. A similar release kinetic was observed with HMA. Supernatants of PSEC-loaded membranes stimulated proliferation. The effect of PSEC-loaded Bio-Gide on proliferation decreased rapidly, as observed in supernatants taken after 3, 6, 24 and 48 hours. Supernatants from Bio-Gide loaded with secretome from unwashed platelets had a stronger impact on proliferation than that from washed platelets. Bio-Gide loaded with HMA induced a strong pro-angiogenic response, which was lower with supernatants taken after 3, 6, 24 and 48 hours. Conclusion: Bio-Gide releases PSEC, OSEC and HMA with a burst-like release kinetic. The ability of PSEC- or HMA-loaded collagen barrier membranes stimulate oral tissue regeneration through their mitogenic and pro-angiogenic effects should be assessed in preclinical studies. -


USE OF 3-D COLLAGEN MATRIX (MUCOGRAFT) IN SURGICAL MANAGEMENT OF ORO-ANTRAL COMMUNICATION (OAC) AND ITS COMPARISON TO OTHER MODALITIES
Objectives: Oro-antral communications (OAC) can occur after extraction of teeth in the maxilla. Several closure techniques can be used to treat the complication, including conservative flapless techniques. The aim of this study was to compare different techniques for closure of OAC and evaluate their efficiencies. Methods: Ninety-five patients with OAC were divided into five groups of 15 patients for treatment with: a flapless technique with Mucograft Sealä/®, a flapless technique with collagen in root design, a Wasmundä/® buccal flap, free-flap from palate, and a sandwich technique (collagen–Bio-Ossä/®-collagen-free gingival graft). In the first 2 weeks after intervention, patients recorded their perceptions of bleeding, swelling, pain and bruising on a visual analogue scale (VAS). Post-surgical complications were assessed clinically at 1 week, 2 weeks, 1 month and 6 months post-surgery. Results: Closure of all wounds was achieved from 2 weeks to 1 month. There were no post-surgical complications. All VAS parameters decreased to almost zero by day 14 and were maintained after 6 months. Scores for swelling and bruising peaked on days 2 and 3, respectively, before decreasing. Conclusions: Using a flap or flapless technique depends on personal choice and skills of the surgeon. The use of Mucograftä/® for closure of OAC is effective and safe, and is associated with low morbidity and no post-surgical complications.









