-


REGENERATION POTENTIAL OF BLOOD MESENCHYMAL STEM CELLS – A SIMPLE PROTOCOL FOR BONE GRAFTS IN MEDICAL OR DENTAL OFFICES AND SOFT TISSUE OR CARTILAGE REGENERATION
Objectives: Mesenchymal stem cells are considered to have a positive impact on tissue regeneration, but they require many manipulations and invasive procedures, such as cell harvesting from bone marrow. This study aimed to evaluate a protocol for using smart blood concentrate in the form of injectable platelet rich fibrin (i-PRF) provides platelets, inflammatory cells and considerable quantities of mesenchymal stem cells from a simple blood withdrawal procedure with a short spin time. Methods: Autologous blood was withdrawn and centrifuged in specific i-PRF tubes at a very low speed for a short time, producing a supernatant of i-PRF. After flow cytometric analysis, specific markers (CD34–, CD45–, CD44+, CD73+, CD90+, CD105+) were applied to detect mesenchymal stem cells. The supernatant was injected into human knee and temporomandibular (TMJ) joints and in sites for soft tissue and bone regeneration within the oral cavity in a total of 40 patients suffering from TMJ and knee joint disorders. Results: Numerous mesenchymal stem cells (0.4–2.0% of total cells) were present in the supernatant. They were cultured in in mono-culture and co-culture with other mesenchymal cells, such as osteoblasts, fibroblasts and endothelial cells. Injection into a graft included clotting of granulesin 1 minute and produced a solid bone graft without any granule mobility (sticky bone graft). Six injections resulted in cartilage regeneration in 10 patients and significant pain relief was achieved in 10 with TMJ dysfunction. In the other 20, better soft tissue and bone regeneration was achieved compared with control groups who received bone substitute and collagen-based materials without i-PRF. Conclusions: This simple protocol may lead to new clinical applications of stem cells for tissue regeneration. The presence of stem cells within the inflammatory milieu might optimise synergy between mesenchymal stem cells and inflammatory cells for soft tissue and bone regeneration. -


EXTRACTED TOOTH ROOTS USED FOR LATERAL ALVEOLAR RIDGE AUGMENTATION—A PROOF-OF-CONCEPT STUDY
Objectives: To assess the efficacy of tooth roots used as autografts for lateral ridge augmentation and two-stage early osseointegration of titanium implants. Methods: The maxillary premolars of foxhounds (n=8) were randomly assigned to undergo either endondontic therapy (PM-E) or be untreated (PM-C). Retromolar cortical autogenous bone (AB) blocks served as controls. PM-E, PM-C and AB were used for ridge augmentation at chronic-type defects in both lower quadrants. After 12 weeks, titanium implants were inserted and left to heal for another 3 weeks. Histological analyses focused on the crestal ridge width (CW), augmented area (AA) and bone-to-implant contact (BIC). Results: Both PM and AB grafts with exposures 3 (AB), 4 (PM-C) and 7 (PM-E) were gradually involved in the bone remodelling process and were associated with replacement resorption. Median crestal ridge widths were 2.70mm (PM-C) vs 3.30 mm (AB) and 2.96mm (PM-E) vs 3.35 mm (AB). For augmented areas they were 7.55mm2 (PM-C) vs 8.56 mm2 (AB) and 11.20mm2 (PM-E) vs 6.60 mm2 (AB). For bone-to-implant contact they were 36.96% (PM-C) vs 64.10% (AB) and 50.79% (PM-E) vs 32.53% (AB). These values were comparable in both PM and AB groups (p>0.05). Conclusions: The extracted tooth roots have structural and biological potential as alternative autografts to autogenous bone. A higher exposure rate may be expected when using endodontically treated teeth. -


BONE EXPANSION WITH SCREWABLE BONE EXPANDERS IN THE AESTHETIC ZONE – A CASE REPORT
Objectives: Ridge-splitting techniques are used in resorbed ridges. They are difficult to perform and highly technique sensitive. In this case report we present a miniinvasive protocol for a safe and reproducible single-implant rehabilitation in resorbed anterior sites. The rationale for our technique is increasing crest thickness with a controlled bone expansion and achieving optimal aesthetic with a safe and simple protocol. Methods: An 18-year-old patient had a traumatic avulsion of the right central incisor due to maxillofacial trauma. Surgical debridement of the contaminated alveolus and socket preservation using deproteinised bovine bone were performed. An epithelial connective graft was sutured to size to cover the bone graft and promote healing by first intention. A Maryland bridge was used for interim restoration during the healing period, using a woven polyethylene fibre, the lost tooth and a flowable composite to define an ovatic pontic profile (BeautifilTM/®). After 4 months the site was healed. The proximal papillae were maintained and moderate resorption in the buccolingual direction was clinically evident. A mini-invasive partial thickness flap was performed to access the bone crest, with an insertion axis determined using a pilot drill. A series of four ( 1.80mm, 2.15mm, 2.50mm, 3.30mm) hand-screwable bone expanders (BTLockTM/® expanders kit) were inserted to increase peri-implant bone density and crest thickness. Bleeding was induced by scratching site walls with the 2.50-mm expander, and a 3.75-mm wide implant was inserted. A connective graft was inserted to reproduce the iugum alveolare and to improve soft tissue aesthetics. The flap was sutured around a composite custom healing cup, reproducing the transmucous tooth morphology and the Maryland was affixed to the adjacent teeth. After 6 months the implant was functionalised with a provisional screwed restoration. Results: Clinical evaluation of soft tissue healing was positive after 4 months from socket preservation. The combination of bone expansion and connective graft was successful in restoring the buccolingual dimension and achieving a natural aesthetic. The use of bone expanders reduced patient discomfort because no cooling system is needed, and improved implant primary stability through their compacting action on peri-implant bone. An adequate pink aesthetic was achieved by using a continuous tissue-conditioning action of interim restorations with an ovatic pontic profile of the Mariland bridge and a tooth-like custom composite healing cap, and surfaces with properties that minimise plaque adhesion (Surface Pre-Reacted GlassTM/®). Proximal papillae were adequately represented during all treatment phases. Conclusions: Bone condensers should be the object of future studies as their use provides a predictable solution for cases that often come to the attention of general dentists but are difficult to treat (even for experienced surgeons). Because they do not need cooling, they are useful in patients with a pronounced gag reflex. They can be used in the posterior maxillary region to increase bone density around implant sites. In this report, they were used in combination with routine periodontal and prosthodontic procedures to treat a mild transversal crest resorption in a highly aesthetic area. -
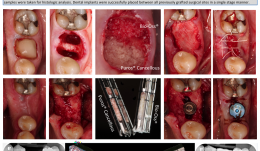

CLINICAL AND HISTOLOGICAL ANALYSIS OF DUAL SOCKET GRAFTING – A PILOT STUDY
Objectives: Extraction socket grafting has been validated for preservation of alveolar ridge dimensions following tooth loss. For making a scientific comparison of different materials requires extraction of at least two teeth. This pilot study aimed to explore the viability of using a single mandibular molar extraction to compare two different materials. The results were evaluated and compared clinically, radiographically and histologically. Methods: Five consecutive patients received an atraumatic tooth extraction of the mandibular first molar with subsequent placement of bone allograft (PurosTM/®) in one socket and xenograft (Bio-OssTM/®) in the other. All sites were covered with a single layer of an absorbable collagen membrane (Ossix PlusTM/®), which was intentionally left exposed. After 20 weeks, the surgical sites were accessed for placement of dental implants. Prior to placement, two trephine core samples were taken for histologic analysis. Dental implants were successfully placed between all previously grafted surgical sites in a single-stage manner. Results: Complete healing of both grafted sites was observed at 20 weeks. The clinical and radiographic aspects of the sites grafted with either allograft or xenograft were significantly different. Xenograft-grafted sites were significantly more radiopaque and residual graft particles were seen at the alveolar crest; allograft-grafted sites demonstrated radiopacity similar to non-grafted adjacent areas, and no visible residual graft particles were seen at the osseous crest, suggesting a higher degree of material turnover. Significant differences were also observed histologically, with more residual graft particles and less vital bone where xenograft was placed, confirming that the two materials behave in significantly different ways when placed in extraction sites for alveolar ridge preservation. Conclusions: This pilot study demonstrated that a single mandibular molar socket can be used to make both clinical and histological comparisons between two different types of bone grafting materials. Future studies should consider using this less traumatic and more convenient research protocol. -
![IN VITRO ASSESSMENT OF PRIMARY STABILITY OF BONE TRUST[TM] SINUS IMPLANT DESIGN—A PRELIMINARY STUDY](https://library.dental-campus.com/media/catalog/product/cache/3/small_image/260x151/17f82f742ffe127f42dca9de82fb58b1/s/i/sinus_implantat.pdf_1_2.png)

IN VITRO ASSESSMENT OF PRIMARY STABILITY OF BONE TRUST[TM] SINUS IMPLANT DESIGN—A PRELIMINARY STUDY
Objectives: The aim of this in vitro study was to analyse the primary stability of BoneTrust Sinus[tm] implant, which suggested to enable higher primary stability by its special design with reduced thread section in cases of reduced vertical bone height, in comparison with standart BoneTrust[tm] implants. Methods: A bone window with dimensions of 3cm x 4cm x 3cm, resembling the maxillary bone window of the lateral sinus wall, with a 4-mm residual bone height was prepared at the dorsal side of freshly slaughtered bovine ribs. Each bone window was fitted with either a BoneTrust Sinus[tm] implant (Sinus) or a Standard BoneTrust[tm] implant (Standard) with the same diameter (either 4mm or 5mm). After implant placement, the international stability quotient (ISQ) was measured by using radiofrequency analysis (RFA) with the Osstell device. Results: A total of 88 implants were placed. ISQ values were 71–84 (Sinus) and 64–80 (Standard) with diameters of 4mm, and 63–78 (Sinus) and 64–80 (Standard) with diameters of 5mm. Among the implants with 4-mm diameters, all Sinus implants showed higher ISQ values than Standard implants (p Conclusion: Within the limitations of this in vitro study using bovine ribs as an experimental model, higher implant primary stability was found for the BoneTrust Sinus[tm] implants with a 4-mm diameter compared to Standart BoneTrust[tm] implants. The use of BoneTrust Sinus[tm] implants with a diameter of 4mm may be associated with higher ISQ values during simultaneous implant placement in conjunction with lateral sinus floor augmentation as suggested by the manufacturer. -


PROTEASE-ACTIVATED RECEPTOR-1 AND PERIODONTAL TISSUE REPAIR
Objectives: Protease-activated receptor-1 (PAR-1) activation by thrombin may play a role in bone growth, repair and homeostasis of periodontal tissues. The aim of this study was to investigate PAR-1 expression in patients with periodontitis, before and after non-surgical periodontal treatment, and relate its expression with the presence of inflammatory biomarkers. Methods: Gingival crevicular fluid (GCF) samples were collected and clinical evaluations made (probing depth, clinical attachment level, bleeding on probing, gingival and plaque indices) in periodontally healthy subjects and patients with chronic periodontitis (CP) at baseline and 6 weeks after periodontal treatment. PAR-1 mRNA expression at the GCF was evaluated by qPCR. Flow cytometry analysis identified the PAR-1-expressing cells. GCF inflammatory biomarkers were also assessed. Results: After periodontal treatment, clinical parameters were significantly improved (p Conclusions: Periodontal treatment resulted in PAR-1 overexpression in the GCF, and PAR-1 expression was inversely associated with the expression of inflammatory biomarkers in the GCF. Thus, the data suggest the importance of PAR-1 mediating the known anabolic actions of thrombin in the periodontium. More studies are necessary to elucidate the mechanism of PAR-1 on periodontal tissue repair. -


WHEN THINGS GO WRONG AFTER SINUS FLOOR ELEVATION
Objectives: Lateral sinus floor elevation (LSFE) is a procedure that allows insertion of dental implants in severely atrophic alveolar ridges in posterior maxilla. Early failure is possible during the osseointegration period and late failure is possible during loading, due to chronic inflammation. Additional LSFE is sometimes needed to restore normal chewing function. We present a case series in which additional LSFE was successfully performed after the occurrence of early and late complications. Methods: In four patients treated in the Department of Maxillofacial and Oral Surgery at the University Medical Centre Ljubljana, four implants were inserted in the posterior maxilla with LSFE using deproteinised bovine bone mineral (DBBM; Bio-OssTM/® and collagen membrane Bio-guideTM/®). Three implants were simultaneously inserted during LSFE. In one patient, implants were inserted 4 months after LSFE. Three implants in three patients were removed during re-entry and placement of healing abutments. The fourth implant was fractured after 5 years of function due to undiagnosed and untreated peri-implantitis. Lost implants in three patients were removed, the implant sites were debrided, and the wounds left to heal for 4 months. Then the fractured implant was partially removed. The apical part was osseointegrated and left in place. In two patients, oro-anthral fistula developed, which was closed by advancement of buccal flap. After healing for 4 months, cone-beam CT was performed and additional LSFE was done in all four patients with simultaneous implant placement with deproteinised bovine bone mineral (DBBM) and collagen membrane. In three patients, fibrous encapsulation of DBBM was found and removed and purulent discharge occurred in two patients. Antibiotics, decongestants and analgesic therapy were given to all patients in the postoperative period. Results: Mean alveolar ridge height before additional LSFE was 3.8mm (range 4.0–3.5mm). In all patients, the Schneiderian membrane was intact during the second elevation. All implants osseointegrated uneventfully. Healing abutments were inserted after 4 months of healing and prosthetic constructions were delivered according to a standard prosthetic protocol. Conclusions: Despite the fact that LSFE is predictable, failures can occur. With a proper surgical protocol in place, additional LSFE can be performed once again. During the second LSFE, all infected DBBM particles have to be removed and the integrity of Schneiderian membrane must be maintained. -


THE EFFECT OF BIOENGINEERED MUSSEL GLUE AS A bone morphogenetic protein (BMP)-2 CARRIER FOR BONE REGENERATION
Objectives: Recombinant human (rh)BMP-2 is known to induce bone formation by stimulating osteoblast differentiation. Mussel adhesive proteins (MAPs) secreted from mussels have been suggested as suitable adhesives for tissue engineering and medicine. In this study, rMAP was used to immobilise rhBMP-2 on a titanium mesh (Ti-mesh) surface, and the osteoinductivity of the BMP-2/rMAP on Ti-mesh surfaces was investigated in vitro and in vivo. Methods: (i) Expression and purification of rMAP: Hybrid rMAP was expressed in Escherichia coli and the proteins were harvested for purification after centrifugation. The rMAP was extracted using 25% (vol/vol) acetic acid, and endotoxin was removed by sequential purification. The purity of rMAP was assessed by 12% (wt/vol) sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). (ii) BMP-2 immobilisation using rMAP on Ti-mesh surfaces: For in vitro analysis, surfaces were coated with 50µg/cm2 of rMAP solution after removing all organic molecules from the Ti-mesh surface. To immobilise BMP-2 on Ti-mesh surfaces, rMAP solution was mixed with 50µg/mL of rhBMP-2 in sodium bicarbonate (pH 0.8), and coated on the mesh surfaces as described previously. (iii) Animal surgery for in vivo bone regeneration ability assays: Each kind of Ti-mesh surface was tested on male Sprague-Dawley rats (n = 6) weighing 250–300g. The rat calvaria were exposed through skin and periosteum incisions using a #15 surgical blade, and circular bone defects were punched using a 8-mm diameter trephine drill under saline irrigation. Two short screws were used to fix each Ti-mesh (prepared just before surgery) over the defect. (iv) Radiographic and histological assessment was made of in vivo bone regeneration. (v) In vitro cell attachment and proliferation assays were performed. (vi) In vitro osteoblast differentiation assays included phenotypic differentiation assays and osteogenic gene expression analysis. Results: Through micro-CT analysis and histological evaluation, the BMP-2/rMAP-coated titanium surfaces displayed improved new bone formation in the rat calvarial defect model compared to rMAP-coated and uncoated surfaces. In addition, cellular behaviours (e.g. adhesion and proliferation) of mouse pre-osteoblast MC3T3-E1 cells were significantly increased on Ti-mesh surfaces coated with BMP-2/rMAP and rMAP. The BMP-2/rMAP-coated surface showed the highest degree of osteogenic differentiation. Messenger RNA expression of osteogenic differentiation marker genes was upregulated in MC3T-E1 cells on BMP-2/rMAP-coated Ti-mesh surfaces. Conclusions: Recombinant MAP is a promising biomaterial for BMP-2 immobilisation on titanium surfaces and guided bone regeneration with enhanced osteoinductivity -


PERI-IMPLANT ALTERATIONS AFTER IMMEDIATE IMPLANT PLACEMENT AND PROVISIONALISATION IN SOCKETS PRESENTING WITH A FACIAL BONE DEFECT WITH SOFT TISSUE GRAFTS—A PROOF-OF-PRINCIPLE STUDY
Objectives: The study aimed to evaluate soft and hard tissue alterations following flapless immediate implant placement and provisionalisation in sockets with a facial bone dehiscence that were reconstructed and received different soft tissue grafts in a proof-of-principle, randomised clinical trial of 1-year duration. The hypothesis was that the use of a soft tissue graft would reduce gingival margin apical migration at the facial aspect. Methods: Twenty-four patients with a single failing maxillary incisor presenting with a facial bone dehiscence were selected. After tooth extraction and narrow implant installation with a torque in excess of 32 N/cm, patients were randomised into three groups (n = 8): a control group (CTL) with no soft tissue graft; a collagen matrix (CM) group using Mucograft[tm]; and a connective tissue graft group (CTG) using subepithelial connective tissue from the palate. Sockets were reconstructed with inorganic bovine bone mineral containing 10% of porcine collagen (Bio-Oss Collagen[tm]) and a non-cross-linked collagen membrane (Bio-Gide[tm]). Additionally, a provisional with a concave subgingival contour an no occlusal contacts was installed in the implants. Clinical, photographic, aesthetic and tomographic analyses were performed by a blinded examiner at baseline, 6 months and 12 months to evaluate tissue alterations. Results: All implants were successfully osseointegrated and a few minor complications occurred. Gingival margin apical migrations of 0.72 ± 0.57mm, 0.42 ± 0.60mm and –0.04 ± 0.3mm occurred respectively in groups CTL, CM and CTG; this was significantly lower in the CTG group than the CTL group. Soft tissue thickness was significantly increased at 12 months for CTL (2.11 ± 0.60mm), CM (2.1 ± 0.54mm) and CTG (3.04 ± 0.61mm. The CTG group demonstrated significantly greater thickness and alveolar ridge contour in comparison to CTL and CM. No significant differences were observed between groups in terms of aesthetic evaluation, papilla apical migration, and height and thickness of the bone in contact with the facial aspect of the implant. In five patients, it was not possible to completely reconstruct the facial bone wall; this was related to the transverse format of the ridge defect, influencing both facial bone height and thickness. Conclusion: Minimal soft tissue alterations occur after immediate implant and provisional placement in sockets with buccal bone dehiscences 1 year after the surgical procedure. The use of connective tissue grafts avoids gingival margin apical migration, and provides better contour of the alveolar ridge and greater thickness of the soft tissue at the buccal aspect of the implant. -


MICROTOMOGRAPHY AND MICROSCOPIC ANALYSIS OF THE BEHAVIOR OF RECOMBINANT BONE MORPHOGENETIC PROTEIN-2 (rhBMP-2) ASSOCIATED WITH BIOMATERIALS IN REPAIRING DEFECTS CRITICS ON RAT CALVARIUM
Objectives: Tissue engineering is a rapidly growing field concerned with providing biological replacement therapies for damaged tissues and organs. This study compared bone formation induced by rhBMP-2 associated with two particulate bone substitutes in critical-size defects in rat calvaria. Methods: Thirty male Wistar rats were divided into six groups of five animals: Group 1 rhBMP-2 (sacrificed after 2 weeks); Group 2 rhBMP-2 (sacrificed after 8 weeks); Group 3 rhBMP-2 + xenogeneic graft (sacrificed after 2 weeks); Group 4 rhBMP-2 + xenogeneic graft (sacrificed after 8 weeks); Group 5 rhBMP-2 + synthetic graft (sacrificed after 2 weeks); and Group 6 rhBMP-2 + synthetic graft (sacrificed after 8 weeks). All samples obtained underwent microtomography (micro-CT) for quantitative assessment of bone growth and descriptive histological analysis. Micro-CT analysis was performed according to the guidelines of Kallai et al. (2011). Results: In the interval between 2 to 8 weeks, group 2, group 4 and group 6 showed a significant increase in bone mineral density. After 2 weeks, group 3 and group 5 showed higher bone mineral density than group 1. After 8 weeks, the rh-BMP-2 alone (group 2) showed higher bone mineral density than groups associated with biomaterials (group 4 and group 6). The percentage of newly formed bone was significantly increased after 8 weeks in the groups in which rhBMP-2 was associated with biomaterials (group 4 and group 6) compared to group group 3 and group 5 after 2weeks. The two evaluation methods used in this study were effective. Conclusion: We conclude that xenogenic material and synthetic graft associated with rh-BMP-2 have the same effect on density and volume of newly formed bone. When used alone, rhBMP-2 can be applied with the same results, with bone growth that is similar to that seen in the groups with biomaterials, and statistically higher bone density than the groups with biomaterials. -


AUTOGENOUS GRAFTS IN BLOCK VERSUS XENOGENEIC GRAFT BLOCK—A CLINICAL STUDY IN HUMANS
Objectives: The aim of this study was to evaluate the stability (bone resorption) of autogenous and xenogeneic grafts in block and the primary stability of implants in the grafted areas. Methods: Eight patients were selected with two defects of bone thickness in the anterior maxilla. A graft of autogenous mandibular branch block was fixed on one side and xenogeneic (Bio-Oss Block[tm]) on the other; both were covered with a collagen membrane (Bio-Gide[tm]). Before and after graft fixation, vestibular–palatal bone thickness was measured on the mesial expanded head-set screw using a thickness gauge. After 6 months, another clinic measure of bone thickness was made in the same place, and a Cone Morse taper Alvim 3.5x10mm implant was placed (Neodent) in each graft. Primary stability was measured with a surgical wrench at the time of implant placement. For tomographic evaluation, tests were performed preoperatively, immediately postoperatively, and 6 months later. CT scans were made of the sagittal graft on the centre of the bone block and of the Bio-Oss Block[TM] and linear measurements were recorded. Results: The mean post-graft thickness at 6 months in autogenous grafts was 7.4mm, with an initial mean of 3.4mm and resorption at 2.6%; for the Bio-Oss Block[tm] the means were 8.9mm and 3.3mm, with resorption of 7.3%. Tomographic analysis at 6 months in autogenous grafts showed mean post-graft thickness of 7.8mm, with an initial mean of 3.7mm, and resorption of 0%. For the Bio-Oss Block[tm] the means were 9.3mm and 3.6mm and 2.1%, respectively. The mean implant insertion torque averaged 32±22N/cm in patients receiving autograft and 18±9N/cm in those receiving xenogeneic grafts. Conclusion: The use of xenogeneic bone graft block achieves a level of thickness and primary stability that indicates successful treatment. -


SOCKET PRESERVATION FOR IMPLANT-SITE MANAGEMENT USING PLATELET RICH FIBRIN (PRF)
Objectives: Traumatic loss of a natural tooth in the aesthetic zone demands immediate attention. One predictable option is socket seal with relined natural tooth, which helps to preserve the gingival parabolic contours and papilla (essential for maintaining natural simulation of soft tissue). Using natural tooth as a socket seal helps to maintain a dentogingival soft tissue collar and initiate a tissue healing process similar to that of tooth replantation. This report describes a patient with trauma-induced loss of an anterior tooth. Methods: The avulsed natural crown was sectioned and used as a socket seal, splinted with the patient’s adjacent teeth. After 3 months, an Ankylos[tm] implant was placed with immediate restoration over the final abutment using the same natural tooth as pontic. Results: Healing was uneventful, with a good emergence profile and healthy papilla at 3 months before placement of the implant. After follow-up of 6 months, vertical height of papilla and bone-crest-to-bone-contact distance were maintained. Conclusion: Replacement of missing natural tooth in aesthetic zone is always a clinical challenge. Simulating the exact dimensions of the lost tooth – especially on the cervical part of the new provisional restoration – is expected to optimise healing and promote a natural-looking emergence profile. The natural dental crown, connected to an implant instead of the root, is applied for tight sealing of the wound. When a tooth is not available because of a traumatic impact, a naturally dimensioned crown restoration is an alternative wound sealant.









