-


MOLECULAR DISCRIMINATION AND ANGIOGENESIS PROPERTIES OF HUMAN OSTEOBLASTS FROM DIFFERENT BONE ENTITIES
Objectives: Autologous grafts from the iliac crest remain the gold standard for alveolar ridge reconstruction. This study aimed to compare the osteogenic potential of human osteoblasts from alveolar and iliac crest bone. Methods: We compared primary human alveolar osteoblasts (aHOBs) and human iliac osteoblasts (iHOBs) derived from patients undergoing routine intraoral bone grafting. Their proliferation potential was evaluated using real-time impedance monitoring. The relative gene expression of bone-specific biomarkers was determined by quantitative polymerase chain reaction (qPCR). Immunohistochemistry, phase-contrast microscopy, alkaline phosphatase (ALP) assay and alizarin red staining were used to visualise cell morphology and mineralisation capacity. In a second part of the experiment, the angiogenesis potential of OPN (osteopontin) derived from aHOBs and iHOBs was investigated using human umbilical vein endothelial cells (HUVECs) in terms of migration and tube formation. Results: The proliferation rate of aHOBs was nearly twice as fast as that of iHOBs (130 hours versus 80 hours). ALP activity and alizarin staining in both aHOBs and iHOBs indicated similar mineralisation capacities. Expression of seven genes (BMP-1, CSF-1, TGF-BR1, ICAM-1, VCAM-1, OPN and DLX-5) was significantly higher in iHOBs than aHOBs. In line with its gene expression, secretion of OPN was greater in iHOB supernatant than aHOB supernatant. OPN was found to stimulate migration of HUVECs (but not tube formation), confirming its role in angiogenesis. Conclusion: These data suggest that osteoblasts derived from iliac crest have higher osteogenic potential than primary osteoblasts from alveolar bone. This may enhance our understanding of the molecular impact of bone cells from different bone sources on bone regeneration in alveolar ridge reconstruction.Secreted OPN was found to have a role in angiogenesis by stimulating migration of HUVECs. -


RECONSTRUCTION OF 3-D ALVEOLAR DEFECTS BY USING A CUSTOMISED MESH (YXOSS CBR) IN 100 CASES
Objectives: Missing or reduced buccal bone plates, as well as a reduced vertical dimension, still represent challenges in bone augmentation and require 3-D reconstruction. Modern individualised dentistry intends to provide new therapeutic concepts based on computer aided CAD-CAM technology and 3-D printing. The aim of this study was to establish a protocol for the clinical application of a patient-specific titanium mesh (Yxoss CBR9) for customised bone regeneration. Methods: One hundred patients were treated by this technique during a two-year period. A 3-D projection of the bony defect was generated and an individualised titanium mesh was designed using CAD-CAM procedures and rapid prototyping. The meshes were installed using a mixture of autogenous bone graft harvested from various intraoral donor sites and Bio Oss[TM] particles in a ratio of 1:1. Implant placement was simultaneous with mesh insertion, or after a healing period of six months combined with removal of the mesh. Evaluation of mesh size, defect region, augmentation site, healing difficulties and soft tissue management was performed. Results: This technology was able to reproduce the alveolar defect properly and produce adequate dimensional accuracy. In all cases, the mesh was placed easily as designed and 3-D bone augmentation was achieved in a predictable way. No serious complications were seen during the healing period and exposure of the mesh did not lead to augmentation loss. Proper soft tissue management and additional use of BioGide[tm] showed a significantly improved outcome. Implant placement was not possible in two cases due to patient non-compliance. Mesh removal was facilitated and caused no bone loss. Histological analysis revealed well-organised, newly formed bone. Conclusion: This protocol using a customised mesh (Yxoss CBR facilitated and shortened surgery time and improved the quality of rehabilitation processes in bony defects. Augmentation volume was predictable and surgery was less invasive. -
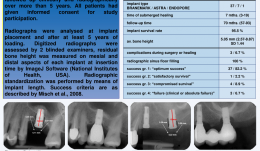

A LONG-TERM RETROSPECTIVE ANALYSIS OF OSTEOTOME SINUS ELEVATION AND SIMULTANEOUS IMPLANT PLACEMENT
Objectives: Twenty years after Summers’ first description of the transalveolar osteotome technique in the posterior maxilla, this procedure is the standard method for sinus floor elevation. Minimal post-operative morbidity, reduced treatment time and lower patient expenses are some of the advantages over the more invasive lateral window approach. The aim of this study was to retrospectively evaluate screw-type implants with simultaneous sinus augmentation placed between 2002 and 2008. Methods: Screw-type implants (n = 45) were placed in molar sites with reduced bone height using the osteotome technique with simultaneous augmentation and deproteinised bovine bone mineral (DBBMc). After a minimum healing time of 12 weeks, implants were loaded with single cemented (porcelain-fused-to-metal) crowns. All patients were followed up clinically and radiographically for more than 5 years. Results: Of the 45 implants, 3 (6.6%) were lost and 37 (82.2%) were in “optimum functional and aesthetic condition”. All implant sites with functioning fixtures showed complete radiographic opacity in the formerly augmented sinus areas. Bone height increased significantly (p Conclusion: Transalveolar sinus floor elevation using graft material leads to successful functional and aesthetic long-term outcomes. -

COMPARISON OF DIFFERENT BONE SUBSTITUTES BASED ON A LITERATURE REVIEW
Objectives: Many procedures require the use of bone grafts to replace or recover the volume of bone that has been resorbed. Many configurations of dental implants exist, along with bone autografts, bone allograft, alloplastic bone substitutes and bone xenograft, to recreate physiological occlusion, and aesthetic and masticatory function. We aimed to investigate whether autogenous bone is still the gold standard for treating patients. Methods: We performed an electronic literature search of the PubMed[tm] database using search terms “substitute bone materials”, “bone grafts”, “bone autografts”, “alloplastic bone”, “bone allograft” and “bone xenograft”. We identified between 100 and 200 research papers and reviews, from which the abstract was read to select 70 (excluding all those that did were not dentistry-related). Qualitative assessment was performed on publications that clearly met the following inclusion criteria: recent papers, published in the last 8 years, related to the terms listed above. Results: The individual healing profile of a given bone substitute with respect to osteogenic potential and substitution rate must be considered when selecting adjunctive grafting materials for bone regeneration procedures. Bone replacement materials could be classified into xenografts, or. substances or other natural hydroxyapatite and biocompatible substances. Allograft materials belong to the same species, but do not contain living cells. Alloplastic materials are synthetic materials used instead of real bone. Autograft bone can be obtained from various intraoral and extraoral sites, such as iliac crest, cranial vault, and tibia of the patient. Different case reports reported the use of different bone substitutes. In one study, standardised mandibular defects in mini-pigs were filled with nanocrystalline hydroxyapatite (HA-SiO), deproteinised bovine bone mineral (DBBM), biphasic calcium phosphate (BCP) with a 60/40% HA/β-TCP (tricalcium phosphate) (BCP 60/40) ratio, or particulate autogenous bone for histological and histomorphometric analysis. At 2 and 8 weeks, the percentages of fillers in the test groups were DBBM 35.65%, HA-SiO 34.47%, and BCP 60/40 23.64%. It was significantly higher than autogenous bone and was substituted more quickly, producing more new bone (17.1% ). These findings suggest that the osteogenic potential of HA-SiO and BCP is inferior to that of autogenous bone. However, if a low substitution rate is desired to stabilise volume, as in the aesthetic zone, then HA-SiO and DBBM may be preferable. Conclusion: Despite the increasing number of available bone substitutes in the last years, bone autografts remain the gold standard. They are osteogenic, osteoinductive and osteoconductive, and the newer ones have a regulatory action. -


DEGREE OF SATISFACTION WITH CHEWING ABILITY IN PATIENTS REHABILITATED WITH IMPLANT-SUPPORTED RECONSTRUCTIONS
Objectives: The aim of this study was to assess the degree of satisfaction of chewing ability among patients treated with fixed partial dentures and/or single crowns supported on dental implants. Methods: The Dental Impact of Daily Living (DIDL) questionnaire was used, which has a dimension for chewing ability, together with a Visual Analog Scale (VAS) for satisfaction values. Interviews were conducted on a total of 183 patients (71 men and 112 women) with a prosthesis in situ for at least one year, placed between 1998 and 2012 at the University of São Paulo. Forty patients had fixed total prostheses and 143 patients had partial dentures and/or single crowns supported on dental implants. To test the association between variables was used Pearson’s chi-squared test. Results: Of those interviewed, 73.2% of patients (52 men) were satisfied with their ability to chew and 85% (34 with total prostheses) reported satisfaction, however there were no statistically significant differences between them and patients treated with partial dentures and/or single crowns and women. Conclusion: The degree of chewing satisfaction of patients treated with total prostheses and men treated with implants was high, mainly because of the stability and comfort of the prosthesis, followed by aesthetics and hygiene. Accurate articulation and aesthetic requirements seem to be not as important for men as they are for women which shows in terms of levels of satisfaction, but the findings are not conclusive. -
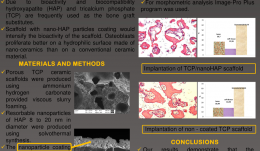

MORPHOMETRIC ANALYSIS OF TRICALCIUM PHOSPHATE (TCP) SCAFFOLDS IN VIVO
Objectives: Trauma and bone pathologies in the maxillofacial region frequently require bone replacement with biomaterials. Due to bioactivity and biocompatibility, hydroxyapatite (HAP) and tricalcium phosphate (TCP) are frequently used as graft substitutes. This study used scaffold with a coating of nano-HAP particles, which intensifies the bioactivity of the scaffold because osteoblasts proliferate better on hydrophilic nano-ceramic surfaces than on conventional ceramic ones. Methods: Porous TCP ceramic scaffolds were produced using ammonium hydrogen carbonate. Resorbable nanoparticles of HAP 8 of 20-nm diameter were produced by solvothermal synthesis, and coated onto the external and internal surfaces of the scaffolds using ultrasonic energy, which ensures strong adhesion of the nanoparticles. New Zealand rabbits (n = 10) were used for in vivo testing. Uncoated and coated TCP ceramic scaffolds were implanted in the lower jaw. Surgically created defects were filled with scaffolds (diameter 5mm, height 3mm). After three months, explanted samples were evaluated for scaffold resorption and bone regeneration. Histology samples were stained with haematoxylin and eosin and evaluated with Leica BME microscopy. Morphometric analysis was conducted using Image-Pro Plus[tm]. Results: Intraosseous implantation of the TCP ceramic scaffold with and without nano-HAP coating initiated new bone formation in all cases. We observed many osteoblasts near the implanted materials as well as rare osteoclasts. Partial destruction of the biomaterial was seen in bone samples. In the uncoated samples, 62.64% of biomaterial remained, with 18.99% newly formed bone and 18.59% soft tissue. In the coated scaffolds, 60.74% of biomaterial remained, with 26.70% newly formed bone and 12.56% soft tissue . Conclusion: The introduction of nano-HAP coating by ultrasonic coating technology can improve the bioactivity of TCP ceramic scaffolds with an increase in new bone formation and have potential for use in maxillofacial surgery. -


IS RIDGE PRESERVATION SAFE OR NOT IN INFECTED SOCKETS? A RETROSPECTIVE DATA ANALYSIS
Objectives: To date, most previous work evaluating healing after tooth extraction has included only fresh extraction sockets. In normal clinic practise, however, the indications for extractions are more complex and certain pathologies are associated with destruction of the socket walls, often resulting in severe resorption. The aim of this study was to evaluate the safety of ridge preservation in infected sockets. Methods: A total of 320 dental records from Seoul National University Dental Hospital archives (January 2011–November 2015) including patients who received extraction due to infection and immediate ridge preservation in the Department of Periodontics were evaluated. the exclusion criteria were as follows: i) ridge preservation in fresh sockets which were extracted due to caries and fracture (excluding retained roots); ii) ridge preservation performed with non-resorbable membrane; iii) age less than 20 years; iv) repetitive medication administration with anti-inflammatory drugs (excluding rheumatoid disease); iv) current pregnancy; and v) history of autoimmune disease. Records were reviewed to identify cases where infection was present (endodontic origin, periodontal origin, and combined endodontic–periodontal origin), which was removed by meticulous debridement and immediately grafted with a biomaterial. The following data were retrieved from the hospital database records: pathologic origin, success and failure rates of the attempted ridge procedure technique, and preservation in infected sockets. Results: A total of 320 ridge preservation surgeries were performed and 13 cases not meeting the inclusion criteria were excluded. Of the 307 eligible subjects, 9 cases (2.93%) were classified as endodontic origin, 198 (64.50%) as periodontal, 90 (29.31%) as combined endodontic-periodontal and 10 (3.26%) unknown. Uneventful healing was observed in 299 sites (97.39%) with no additional medication, whereas six sites (1.95%) needed additional medication (5 days of additional antibiotics) due to inflammatory symptoms. Re-infection occurred in two sites and the biomaterials within the socket were removed. Clinical symptoms included abscess with pus formation, caustic odour, pain and severe bleeding. The cause for failure in site 1 may be attributed to overfilling of the biomaterial attracting new infection source and complicating the closure of the wound. In site2, necrotic bone plate and/or retained root-like radiopacity observed in the CT, suggesting incomplete removal of the infection source within the socket. Besides these two cases of infection, ridge preservation was successful in 305 sites, yielding a high success rate of 99.35%. Conclusion: Within the limitation of this study, our observations suggest that immediate ridge preservation with various biomaterials is a safe procedure, despite the need to graft immediately following tooth extraction and to remove the infection source using the conventional debridement method. Caution is needed when performing debridement so as not to leave root fragments or necrotic bone plates unremoved. Also, overfilling may compromise wound stability at the entrance of the socket and must be avoided for optimum results. -


THROUGH-ROOT IMPLANT SITE PREPARATION FOR ATRAUMATIC EXTRACTION OF ANKYLOSED TEETH IN IMMEDIATE IMPLANT PLACEMENT
Objectives: Immediate implant placement after tooth extraction is widely covered in the dental literature and positive outcomes have been well reviewed and documented, demonstrating that it is a beneficial and predictable procedure for replacing hopeless teeth. The aim of this study was to report two cases of ankylosed teeth extracted with the alternative approach and treated with immediately placed implants. Methods: Two patients presented with ankylosed hopeless teeth, and treated with immediate implant insertion was planned. After local anaesthesia (4% articaine hydrochloride with 1:100 000 adrenaline hydrochloride) without any incision or flap preparation, the first pointer drill was placed into the root canal to thin the root walls without reaching the apex of the tooth. The second pilot drill was placed into the root canal to further thin the walls without passing through the apex. The third drill (using the same pilot drill but with a sterile implant preparation kit) was placed in the root canal, passed through the apex and split the root into parts. Subsequent drills were used to prepare the implant site in the bone passing through the root canal. After mobility of the root fragments was obtained, they were gently separated from alveolar bone using periotomes and removed from the socket with pincettes. The extraction socket was thoroughly curetted before implant insertion. After installation in a palatal position (in avoid traumatising the labial plate of the socket), the buccal gap between the socket wall and the implant was filled with bone grafting material (Bioteck) and a healing screw was installed. The site was sutured to protect the fresh extraction socket and the biomaterial. Results: In both cases it was possible to maintain the integrity of the surrounding bone and obtain primary stability of the implants, and the soft and hard tissue healing processes were uneventful. No peri-implant bone defects were detected by probing around the implants. Radiographic examination of all implants after one year showed no radiotransparency around implants. Our protocol used different drills and a sterile kit during bone preparation to avoid infection by root canal bacteria. Conclusion: Within the limits of a case series, this protocol for extracting and replacing ankylosed teeth with immediate implants seem to be successful. The finding needs to be confirmed by other more statistically reliable studies as randomised controlled trials. Further studies are also needed to confirm the clinical and microbiological advantages of the use of sterile drills at every step. -


EFFECTS OF PLATELET-RICH PLASMA (PRP) PRODUCTS ON VIABILITY AND PROLIFERATION RATE OF HUMAN GINGIVAL FIBROBLASTS (HGF)
Objectives: Platelet preparations are increasingly used to improve bone and soft tissue regeneration, but basic studies are insufficient for supporting the real efficacies of these products. Controversy exists about the effects of platelet product on hard and soft tissue regeneration, therefore more in vitro studies are needed. The aim of this investigation was to compare the in vitro effects of platelet-rich growth factor (PRGF) and platelet-rich fibrin (PRF) on the proliferation of human gingival fibroblasts (HGF). Methods: Whole blood samples were collected from a healthy volunteer. Anitua's PRGF and Choukran's PRF were prepared according to standard protocols. After culture periods of 24, 48 and 72 hours, HGF cell proliferation was evaluated by MTT assay. Statistical analysis was performed using one-way ANOVA followed by Tukey-Kramer’s multiple comparisons and p values less than 0.001 were considered significant. Results: The optical density of the negative control (fetal bovine serum (FBS) 1%) was set at 100% and other groups were expressed as a percentage of this. Our results showed PRGF treatment induced statistically significant (p 1.73%, p Conclusion: PRGF has a strong stimulant effect on HGF cell viability and proliferation compared to PRF. Further comparative studies of PRF and PRGF are needed using more cell lines and primary cells with different in vitro proliferation assays and more in vivo assays. -


THE EFFECT OF FIBRIN-BINDING OLIGOPEPTIDE DERIVED FROM FIBRONECTIN ON MIGRATION OF PERIODONTAL LIGAMENT CELLS IN AN IN VITRO WOUND HEALING MODEL
Objectives: The aim of this study was to evaluate the effect of synthetic FN fragments containing an N-terminal fibrin-binding domain on migration of human PDL fibroblast cells in an in vitro wound-healing model. Methods: Three types of synthetic oligopeptides (FF1, FF3 and FF5; including fibrin-binding domain FN) were allocated to the experimental groups. Recombinant oligopeptide (F20) including type Ш 9–10 domains of FN was as a positive control, and a group treated with nothing was the negative control. Cell migration capacity was evaluated using an Cell Migration Assembly kit. Results: The migration rates and number of migrated cells increased in the test group and both control groups at each point in time (6, 12, 18 and 24 hours). The F20 (positive control) group showed a significantly greater cell migration rate than the control group at 6 and 12 hours (but not at 18 or 24 hours). There were no significant differences among the test groups or between the test and positive control groups (F20) (p Conclusion: Within the limits of this study, the N-terminal fibrin-binding domain of FN was observed to promote cell migration of PDL fibroblast cells. -


BONE-REGENERATIVE ACTIVITY OF PARATHYROID HORMONE (PTH)-RELEASING NANO-HYDROXYAPATITE/POLY(L)-LACTIC ACID (PLLA) HYBRID SCAFFOLDS
Objectives: The study aimed to fabricate a novel bone-regenerative scaffold based on systematic combination of porous organic–inorganic hybrid scaffolds and recombinant human parathyroid hormone (rhPTH). Methods: The hybrid scaffold was fabricatedby immobilisation of polyphosphate-functionalised nano-hydroxyapatite (PP-n-HAp) on the surface of porous poly(l)-lactic acid (PLLA) scaffolds. This was followed by rhPTH loading on the polyphosphates of n-HAp surfaces. The surface polyphosphate functionalities of PP-n-HAp enabled stable chemical immobilisation of n-Hap on the amine-treated pore surface of the PLGA scaffolds. RhPTH with a positive charge was bound at a high efficiency of 98.1–99.5% onto the anionic polyphosphates of PP-n-HAp immobilised on PLLA surfaces and was released sustainably for up to 50 days. The release rate was manipulated by adjusting the amount of loaded rhPTH, and the release data were moderately fitted to the Higuchi’s diffusion model. Results: Immobilisation of PP-n-Hap was performed with a 1-ethyl-3-(3-(dimethylamino)propyl)carbodiimide (EDC)-mediated coupling reaction between the acidic PP groups and the primary amine groups on the surface of amine-functionalised PLLA scaffolds. They have a mean surface pore size of 110±10μm. Even after PP-n-HAp immobilisation, the initial interconnected pore structure and pore diameter were maintained. The pore size of PP-n-HAp-PLLA scaffolds may allow the spaces enough forthe growth of bone-forming cells. Thermogravimetric analysis (TGA) showed that the amount of immobilised n-HAp on the pore surface of PLLA scaffolds was 11.3 wt%. The dose-dependent sustained release patterns of rhPTH from PP-n-HAp-PLLA scaffolds were confirmed by a release profile. Four types of scaffolds were tested in rabbit calvaria defect models: (i) PLLA only, (ii) PP-n-HAp-PLLA, (iii) rhPTH (2mg) loaded PP-n-HAp-PLLA, and (iv) rhPTH (10mg) loaded PPn-HAp-PLLA. After 5 weeks, rhPTH-loaded PP-n-HAp-PLLA (with 2mg and 10mg rhPTH) displayed higher bone growth than the control group (PLLA only). Conclusion: We described the fabrication of porous PLLA scaffolds with rhPTH-releasing PP-n-HAp for bone regeneration. This hybrid scaffold was prepared by PP-n-HAp immobilisation onto the PLLA scaffolds, followed by the sequential rhPTH loading on PP-n-HAp. RhPTH was incorporated with high efficiency, and the sustained release of rhPTH from the hybrid scaffolds was observed for up to 50 days. In the animal experiment, we showed that the pore surface of the PLLA scaffolds had a synergistic bone-forming effect, not only due to surface-exposed osteoconductive n-HAp but also due to the sustained release of rhPTH. This bone-regenerative hybrid scaffold may find broad applications as a bone generation material. -


BONE GROWTH ON TITANIUM IMPLANTS AFTER ELECTRICAL STIMULATION
Objectives: The aim of this study was to measure the contact area of the bone–implant interface on implants submitted to different electric currents. Acceleration of healing time by electric stimulation in animals is still controversial, although several authors have demonstrated that electricity can stimulate bone formation around dental implants, depending on the intensity and period of the impulse as well as the treatment period. Methods: Ninety titanium dental implants measuring 6 mm x 11.5mm and with machined surfaces were used study. They were sterilised using gamma rays. Six male Beagle dogs approximately 12 months old and weighing 15kg were divided randomly into two groups for evaluation at 7 days and 15 days (three animals each time). Three levels of electrical stimulation were delivered to the implants (10μA, 20μA; control 0μA) through an electrical device coupled to the implant connection area. Results: No statistical differences was found in the contact area at the bone–implant interface after for 7 days of electrical stimulation. However, a significant higher contact area was recorded for stimulation at 20μA compared to 10μA and controls (p 0.05). Conclusion: The electrical stimulation of dental implants can increase the contact area at the bone–implant interface due to bone formation. The effect of different electrical current intensities and periods should be studied further to clarify the potential of this method.









