-


SOFT-TISSUE VOLUME GAIN AROUND DENTAL IMPLANTS USING AUTOGENOUS SUBEPITHELIAL CONNECTIVE TISSUE GRAFT FROM THE PALATE OR TUBEROSITY—PRELIMINARY RESULTS OF A RANDOMISED PROSPECTIVE CLINICAL STUDY
Objectives: The main goal of this study was to compare the soft-tissue volume gain around dental implants with subepithelial connective tissue grafts (SCTG) originating from either palate or the tuberosity. The secondary goal was to compare changes in clinical parameters: plaque index (PI), bleeding on probing (BOP), probing depth (PD) and width of keratinised tissue (KT). Methods: Patients with single tooth implants already osseointegrated and in need of soft tissue augmentation were recruited (n = 12) and randomly received an SCTG from the palate (control group) or tuberosity (test group). Recipient sites were prepared by an intracrevicular incision at the buccal side extending to one adjacent tooth on each side, before raising a partial-thickness flap. Grafts of standarised dimensions were stabilised to the buccal flap and closure was achieved without tension. In order to examine volumetric tissue changes, an intraoral optical scanner was used to take two optical impressions at baseline and again 3 months after surgery. Digital software was used to superimpose the stereolithography (STL) files and calculate volume gain. Volumetric changes were calculated at three levels below the healing abutment on the buccal side of the implants (at 1.3mm and 5.0mm). The secondary outcomes were evaluated at baseline and at 3 months. Differences between control and teset groups were calculated for the quantitative variables using the Student’s t-test or Mann–Whitney test (depending on the normality of the distribution) and Chi-squared test for the qualitative variables. A p value of Results: No significant differences in baseline defect size were observed between groups. At 1mm volume gain was 1.28 ± 0.89mm for palate grafts (controls) and 1.28 ± 0.83mm for tuberosity grafts(p=0.39); at 3mm it wasoriginal, 84 ± 1.21mm for palate and 1.1 ± 0.4mm for tuberosity (p=0.31); and at 5mm it was 0.66 ± 0.23mm for palate and 0.95 ± 0.48mm for tuberosity (p=0.39). No statistically significant differences were observed at any level. The tuberosity grafts had a higher volume gain with a mean gain of 1.12 ± 0.57mm (versus a mean gain of 0.88 ± 0.94mm for palate), but these results were not statistically significant (p=0.42). Similarly, there was a tendency for higher KT gain for the tuberosity group, with an increase of 1.16 ± 0.98mm, versus 0.66 ± 0.82mm (p=0.36). A statistically significant reduction in PI was observed for the controls, from 18.0 ±0.89% to 16.3 ±1.03% (p=0.01), but only a slight (non-statistically) significant increase was seen in the test group. Non-statistically significant differences were also observed for PB and BOP. Conclusion: The main goal of this study was to compare the soft-tissue volume gain around dental implants using SCTGs of the same dimensions from either palate or tuberosity. Although the present data is only preliminary, procedures were effective in increasing volume gain around the implants at 3 months. Differences were statistically non-significant, but there was a tendency for increased volume gain with SCTGs from the tuberosity (1.12±0.57mm) compared to palate (0.88±0.94mm). Furthermore, there was a tendency towards for greater KT gain in the tuberosity group (1.16±0.98mm versus 0.66±0.82mm in the palate group). -


ANTIBODY-MEDIATED OSSEOUS REGENERATION (AMOR) IN THE RECONSTRUCTION OF ALVEOLAR RIDGE DEFECTS
Objectives: The aim of this study was to examine the efficacy of antibody-mediated osseous regeneration (AMOR) in conjunction with two novel extraction devices, namely a SocketKAP™ (for obturation of socket orifices) and SocketKAGE™ (for providing space in sites with facial dehiscence for ridge preservation and augmentation procedures following tooth extraction). Methods: In this prospective controlled study, 8–12-year-old macaques (Macaca fascicularis; n = 6) underwent removal of both maxillary and mandibular second left and right premolars (ULPM2, URPM2, LLPM2, LRPM2), both maxillary and mandibular second left and right molars (ULM2, URM2, LLM2, and LRM2) on each side. This was followed by resection of the entire facial alveolar wall. They were randomly assigned to the following intervention groups: dehiscence socket unfilled and uncovered (group A; negative control); dehiscence socket reconstructed with SocketKAGE™ and covered with SocketKAP™ (group B); dehiscence socket reconstructed with SocketKAGE™ and ABBM and covered with SocketKAP™(group C); dehiscence socket reconstructed with SocketKAGE™ and chimeric anti-BMP-2 monoclonal antibody (mAb) and covered with SocketKAP™(group D); dehiscence socket reconstructed with SocketKAGE™ and iso-type-matched control mAb (Iso-mAb) and covered with SocketKAP™ (group E). At 6 and 12 weeks post-extraction, cone beam CT imaging was performed. All files were imported to Simplant TM/® software (for linear measurement of remaining bone width and height at 1mm, 2mm, 3mm and 5mm from alveolar crest) and to reverse engineering Geomagic ControlTM/®software (for volumetric analysis of alveolar bone). Histologic evaluation was also made of the dimensional changes in dehiscence defects after ridge preservation using different materials. Non-parametric analysis of variance was conducted using the methods of Brunnner and Langer. Results: The result from linear and volumetric analyses demonstrated that group D (chimeric mAb +SocketKAP™ + SocketKAGE™) was associated with significantly greater percentages of remaining bone width and height at the buccal point, and remaining bone volume at 6 and 12 weeks when compared to group A (negative control), group B (SocketKAP™ + SocketKAGE™) and group E (Iso-mAb); the latter lost approximately 70% of crestal bone width at the crestal 1 mm point, and ABBM failed to prove more effective in preserving alveolar bone width at crestal 1mm (36%). When anti-BMP-2 mAB was used, the percentage of bone width was as good as those with ABBM at crestal 2mm, 3mm and 5mm areas. However, the most important finding was that the data demonstrated that bone remodelling using chimeric mAb was not only limited to the crestal 2–5-mm zone, but also the crestal 1-mm area, with mean remaining bone widths of 52% and 68% at 6 weeks and 12 weeks, respectively. Both CB-CT and volumetric analysis revealed more active and extensive bone regeneration of marginal bone with chimeric mAb compared to other groups. Histologic analysis showed the knife-edge of alveolar crest following tooth extraction in groups A, B, C and E, as well as statistically significant more bone remodelling in chimeric mAb, including a higher percentage of bone formation within newly generated tissue together with signs of osteogenic cell activity. Conclusions: These results suggest that chimeric anti-BMP-2 mAb, in conjunction with SocketKAPTM/® and SocketKAGETM/® was effective in the reconstruction of the alveolar bone in extraction sockets with facial dehiscence defects. These favourable results may be attributed to advantageous nature of AMOR, such as using endogenous BMP-2 captured by chimeric mAb enhance osteogenesis, with higher biological activity of endogenous BMP and a longer half-life of captured BMP compared to ABBM (which only exhibits osteoconductivity). -
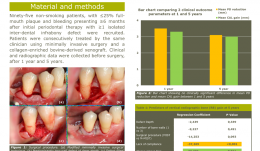

LONG-TERM OUTCOMES OF PERIODONTAL REGENERATION USING A COLLAGEN-ENRICHED, BOVINE-DERIVED XENOGRAFT IN A LARGE COHORT
Objectives: To evaluate the 5-year clinical outcome of regenerative periodontal therapy (RPT) using minimally invasive surgery and a collagen-enriched bovine-derived xenograft (1), and to identify predictors for gains in clinical attachment level (CAL) and vertical radiographic bone (RB) (2). Methods: Subjects were 95 non-smoking patients, with up to 25% full-mouth plaque and bleeding presenting at least 6 months after initial periodontal therapy with more than one isolated interdental infrabony defect. They were treated consecutively by the same clinician with combined surgery and xenograft. Clinical and radiographic data were collected before surgery, and after 1 year and 5 years. Results: Eighty-four patients (39 men, 45 women, mean age 53 years) were available for follow-up after 1 year and demonstrated a mean probing depth (PD) of 7.8mm, a CAL of 10.0mm and a defect depth of 5.2mm before surgery. Thirteen patients dropped out between year 1 and year 5. At 5 years, mean PD reduction was 3.3mm (SD 2.2 ), CAL gain was 3.0mm (SD 2.1) and RB gain was 57% (SD 38). Of these, 45% showed ≥4.0mm CAL gain, and 24% were considered failures (≤ 1.0mm CAL gain), 48% showed considerable RB gain (≥75%).The only predictor for CAL gain included sites that were always plaque-free during aftercare (p= 0.003). Predictors for RB gain included patient compliance (p=0.001) and sites that were always plaque-free during aftercare (p=0.010). Conclusions: Regenerative periodontal therapy using minimally invasive surgery and a collagen-enriched bovine-derived xenograft demonstrated favourable clinical and radiographic outcomes after 5 years. Oral hygiene and patient compliance had a significant impact in the long term. -


REHABILITATION OF A FIBULA-RECONSTRUCTED MANDIBLE BY USING COMPUTER ASSISTED IMPLANT SURGERY. A CASE REPORT.
Objectives: Reconstruction of mandibular integrity following a block resection is complicated by the loss of function and integrity of the graft. We report on rehabilitation of a patient who underwent mandibular resection and fibular reconstruction. Methods: A 16-year-old girl was referred to the Oral Implantology Department Clinic at the Istanbul University Faculty of Dentistry, 2 years after mandibular construction via a fibular graft. The geometry and topography of the graft was inconsistent and challenging for a removable prosthesis. To avoid the risk of fracture and necrosis, computer-assisted planning and flapless implant surgery was chosen as the best course of action. After obtaining a cone beam computerised tomography (CBCT) scan of the mandible with a radiographic template, the images were transferred into dedicated software and three implants were planned for shortened fixed composite–hybrid prostheses. Following surgery, one implant was found to be mispositioned and removed the following day. Results: The mandible was successfully restored by two implant-supported hybrid prostheses, fabricated with the use of nano-filled composite following the osseointegration period. Conclusions: Rehabilitation of a pathologically reconstructed edentulous jaw may be successfully completed using computer-assisted planning and guided implant surgery. Clinicians should be cautious regarding deviations related to the use of sterolithographic guides. -


PERI-IMPLANT BONE REACTIONS TO DIFFERENT IMPLANT MACROSTRUCTURE AND NECK CONFIGURATIONS—A 5-YEAR STUDY WITH 494 IMPLANTS
Objectives: After implant placement, bone remodelling can be observed along the entire implant, but it is more dominant at the level of the implant neck. To date, there have been few long-term studies on the effectiveness of different implant necks and macrostructures for preserving marginal bone. The primary endpoint of this study was to clinically investigate the influence of different implant macrostructure and neck configurations on peri-implant marginal bone loss. Methods: Cylindrical and tapered implants were compared. Statistical analysis was performed using IBM SPSS version 20. Descriptive analysis included the number of implants and mean marginal bone loss for all groups. Results: Cylindrical implants with an external hexagon connection(n=321) featured the greatest marginal bone loss (distance between implant shoulder and bone crest (DIB) 2.341mm ± 1.184). Cylindrical implants with an internal hexagon connection(n=86) displayed less marginal bone loss compared to external connections with the same macrostructure (mean DIB 2.193mm ± 1.121). In contrast, tapered implants with an external hexagon (n=33) showed less bone loss (mean DIB 1.422mm ± 1.063) than those with an internal hexagon (n=54) (mean DIB 1.951mm ±0.793). Statistically significantly differences were found between external hexagon implants with different implant macrostructures. Conclusion: There was a trend for peri-implant marginal bone loss to be directly affected by implant macrostructure. Tapered implants may lead to less marginal bone loss after 5 years compared to cylindrical implants, and may be considered as safe and predictable alternatives. -


Total reconstruction after closure of maxillary sinus fistula
Dr. Thomas TruningerBefore starting the full-mouth reconstruction, the oral-maxillary sinus fistula (oroantral fistula) has to be closed. -

Save the Date: International Osteology Symposium 2016 in Monaco
Osteology returns to a beautiful location: from 21-23 April 2016 the International Symposium will once more take place in Monaco. The International Osteology Symposium is a congress held every three years. The Symposium focuses on bone and tissue regeneration and has gained a reputation for high level science, first class speakers and extensive practice-oriented training. It is also well known for its beautiful congress locations and attractive social events. The program and further information will be published soon. In the meantime, save the date and enjoy the impressions from the International Osteology Symposium in 2013! Photogallery Congress movie -


Osteology Foundation goes social
Through social media its now easier than ever to follow what interests you, to stay up to date with the latest trends and news, and to share with friends and collaborators what might be interesting for them or to find out what they think. The Osteology Foundations official profiles help followers to stay in contact with the community and to keep interested researchers and practitioners, as well as partners from industry, universities and associations, informed about the latest activities and news. Check out the Osteology Foundations profiles on Facebook, Google+, Twitter and LinkedIn and make sure you Like and Follow us to receive always the latest updates, deadlines and news! See you there! -


Osteology Monaco 2016 - we are online!
We are excited to announce that today the website for the International Osteology Symposium 2016 in Monaco went online! Discover the exciting programme under the motto Learning the WHY and the HOW in Regenerative Therapy with international top speakers, as well as all other important information concerning our Symposium. ► Osteology Monaco online check it out! The website will be updated continuously, and you will find the latest information there. Through the website, and all other communication channels, such as E-mailings, Social Media and our Website, we will keep you always informed about updates and approaching deadlines. Online registration on the Osteology Monaco website will open in October 2015. -


Meet Osteology at the Europerio in London
Not long until the EuroPerio 8 Congress in London starts. And Osteology will also be there with the latest news about the Osteology Symposium 2016 in Monaco, new funding possibilities for researchers - and a sweet surprise... The EuroPerio Congress has established itself as one of the worlds leading conference in periodontology and implant dentistry, and has become a triennial fixture on the meetings calendar. The 2015 meeting takes place in London, and is hosted by the British Society of Periodontology for the European Federation of Periodontology. Up to 10000 delegates are expected. The organizers have put together an impressive program with to 6 sessions will run in parallel throughout the meeting. The Osteology Foundation will be present at the congress with its own booth in the exhibiton area, presenting the latest news about the preparations of the Osteology Symposium 2016 in Monaco, new funding possibilities for researchers that will be available soon - and a sweet surprise... Dont miss the chance, and see us in London at booth No. 52b Final program Europerio website Press Conference For representatives of the media an Press Conference will take place during the EuroPerio 8 in London. Registration Further information -

Osteology Press Conference in London
The Osteology Foundation revealed numerous innovations and plans at a press conference held as part of the 8th EuroPerio Congress in London. Announcement of the scientific program for the International Osteology Symposium 2016 in Monaco was one of the highlights. Interesting for scientists undertaking research on oral regeneration are the Foundations new Large Clinical Grants, which were officially unveiled for the first time in London. The changes at the top of the Osteology Foundation were another focal point and provided an ideal opportunity for reviewing the recent years, but also for looking forward to the future and the Foundations strategic advancement. The Osteology Foundation, which was founded in 2003 by Dr Peter Geistlich and Geistlich Pharma AG in Switzerland, has continuously developed and has grown significantly since its inception. Linking Science and Practice Under the motto Linking Science Practice in Oral Regeneration, the Foundation now essentially comprises four key areas in which it is active, Professor Christoph Hmmerle explained in London: Support for researchers, education for practitioners, training for scientists and best practice in science. An independent Foundation Board comprising 12 internationally renowned experts maps out the strategy and activities, explained Hmmerle. The Board is split into three committees (Science, Training, Communication), operatively headed by an Executive Board of four, and it is supported by an Expert Council with 33 members from 13 countries, Hmmerle continued. Change after 12 years Christoph Hmmerle was President of the Foundation since it was established 12 years ago. His period of office ended at the end of May 2015. His successor, Professor Mariano Sanz, takes office from June 2015, with whom the Foundation is in the best hands, Hmmerle stressed. Sustainable growth and continuous development According to Mariano Sanz, under Christoph Hmmerles leadership the Foundation succeeded in becoming well known for the highest quality in science and also in practice. I dont intend to change anything, but will continue to pursue the set course and work to raise the profile of the Foundation, as well as to drive forward its geographical expansion, Sanz announced in London. Here it will be important, he explained, to focus more on new technologies and media to further assure sustainable growth and continuous development. Along with the change at the top, there are other personnel changes at the Osteology Foundation: Myron Nevins, Friedrich Neukam and Massimo Simion will step down from the Foundation Board when their terms of office end. Their successors are Pamela McClain, Frank Schwarz and Istvan Urban. Stronger together Osteology collaborations Collaborations, such as those with the European Federation of Periodontology (EFP), the organisers of the EuroPerio Congress, are of enormous importance to the Osteology Foundation, Sanz explained. Both sides can profit from the partnership. Together we are stronger, he stressed. As a prime example for the successful cooperation, Sanz cited the 10th EFP Consensus Workshop, which took place in collaboration with the Osteology Foundation. The proceedings resulting from the workshop are of great relevance and the publication has been met with keen interest among practitioners, Sanz pointed out. Additional collaborations are in progress worldwide with various professional societies, such as the American Academy of Periodontology (AAP) in North America, the Chinese Stomatological Association in Asia, the IberoPanamerican Federation of Periodontics (FIPP) in Latin America, as well as the Association for Dental Education in Europe (ADEE). Congress highlight in 2016: International Symposium in Monaco In his role as Chair of the Education Committee, Mariano Sanz also introduced the scientific programme for the International Osteology Symposium 2016 in Monaco. Over 2500 participants from 60 countries are expected at the congress, which is held every three years and for many is a notable event in the congress calendar. The Scientific Chairmen of the congress are Friedrich Neukam and Myron Nevins. No fewer than 85 internationally renowned speakers will discuss the most important topics surrounding oral regeneration and the latest insights from science for use in practice, Sanz explained. The programme will be supplemented by a large poster exhibition, practical and theoretical workshops, as well as the Master Clinician Courses held for the first time. The latter are included in the registration fee. Registration will open in October 2015 via the websitewww.osteology-monaco.org, as Sanz confirmed. Abstracts for posters and the Research Forum, for which the best research work presented will be awarded prizes, are welcome from 1 July 2015. New for established research groups: Large Clinical Grants Also when it comes to promoting science, which is one of the Osteology Foundations core tasks, there was exciting news to report, which is probably mainly of interest to the established research groups. Professor William Giannobile, Chair of the Scientific Committee of the Foundation, introduced the Large Clinical Grants, which scientists can apply for in 2015 for the first time. The Large Clinical Grants are worth up to 350,000 Swiss Francs for a maximum project duration of three years. Detailed information for application can be found on the Foundations website from July 2015 on. The application deadline is 1 December. Another new feature of scientific promotion are the Osteology Research Scholarships, which offer up-and-coming researchers a one-year stay at one of the Osteology Scholarship Centres. The first round of applications in 2015 is already over, said Giannobile. But applications can be submitted again from July onwards. The application deadline for the next round is 1 December 2015. Besides the new funding opportunities, the established Young Researcher Grants and Advanced Researcher Grants are still on offer, William Giannobile clarified. Comprehensive information on these grants, aimed towards scientists on different rungs of the career ladder and varying in their level of experience required, may also be found on the Foundation website at www.osteology.org. Career milestones: Osteology Research Academy Professor Reinhard Gruber, another member of the Osteology Board of Trustees, presented the Osteology Research Academy. This is an intensive course lasting several days in which prospective scientists are taught research practice and methodology. More specific research topics pertaining to bone generation are also addressed in an Expert Module. An essential aspect of the courses is the informal atmosphere and the direct contact with experienced scientists, which is much appreciated by the participants, Gruber explained. Questions are discussed and case studies examined in small groups. The concept is met with great interest the world over, according to Gruber. Last years course participants came from 15 different countries on four continents, he recounted. That is a perfect way of establishing new contacts and networks. After the course, one of the participants enthused that the course had changed his life, Reinhard Gruber recalled. Another participant looked back at the courses as milestones in his scientific career. This participant feedback is the best sign that we are on the right track with our course concept. That is why we are also planning to stage the Research Academy in North and South America in the coming years, Reinhard Gruber declared. Professor Christoph Hmmerle at the Osteology Press Conference in London Presenting the key activities of the Osteology Foundation Professor Mariano Sanz talked about the successful collaboration with the EFP Mariano Sanz also presented the programm of Osteology Monaco 2016 - the international symposium next year. Professor William Giannobile described what the Osteology Foundation has to offer for scientists Professor Reinhard Gruber presented the Osteology Research Academy The four Board Members as well as Kay Horsch, Executive Director of the Foundation, were answering questions after the presentations For representatives of the media: Download Press Releases -


Osteology Monaco 2016 - call for abstracts!
The application for Poster Presentations and the Research Forum is open! We invite investigators within the field of regenerative dentistry and dental tissue engineeringto submit abstracts. Deadline is 1 December 2015.The three best Research Forum presentations in each category will be awarded. More information Application form










