-
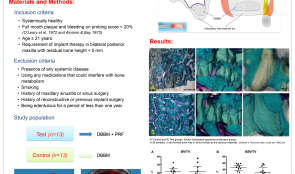

MAXILLARY SINUS AUGMENTATION WITH PLATELET-RICH FIBRIN (PRF) AND DEPROTEINISED BOVINE BONE MINERAL (DBBM) – A SPLIT-MOUTH HISTOLOGICAL AND HISTOMORPHOMETRIC STUDY
Objectives: To evaluate the effect of platelet-rich fibrin (PRF) in combination with deproteinised bovine bone mineral (DBBM) on bone regeneration in maxillary sinus augmentation. Methods: Thirteen patients (9 men and 4 women aged 49.92 ± 10.37) were enrolled in the study. Twenty-six maxillary sinus augmentation procedures were performed randomly using combined DBBM and PRF (test group) or DBBM alone (control group) in a split-mouth design. In both groups, a resorbable collagen membrane was used to cover the graft material. After 6months, bone biopsies were harvested from the implant sites for histological and histomorphometric evaluation. Clinical and radiographic examinations were performed pre- and post-operatively. Results: There was no qualitative histological difference in the two groups. Neo-formed bone was in direct contact with the residual material in all cases. The amount of newly formed bone (test group 21.38±8.78%; control group 21.25±5.59%), residual bone substitute (test group 25.95±9.54%; control group 32.79±5.89%), and bone substitute in contact with the newly formed bone were similar in both groups (p Conclusions: Both methods were effective for maxillary sinus augmentation. PRF did not improve regenerated bone as well as graft that was incorporated quantitatively. -
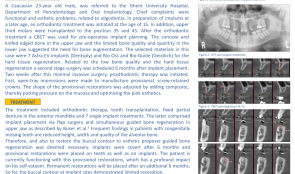

IMPLANT PLACEMENT AND HARD TISSUE REGENERATION FOR OLIGODONTIA AND FOLLOWING ORTHODONTIC THERAPY
Objectives: Tooth agenesis is one of the most prevalent congenital craniofacial disorders. The term oligodontia is generally used for agenesis of six or more teeth, and it can be related to a syndrome or present as an isolated condition. The prevalence in permanent dentition is 0.14%. This article reports a case of oral rehabilitation using implants and hard tissue regeneration in a patient with agenesis of 15 permanent teeth and following orthodontics. Methods: A 23-year-old Caucasian man, was referred to the Department of Periodontology and Oral Implantology at Ghent University Hospital. His chief complaints were functional and aesthetic, related to oligodontia. Orthodontic treatment was initiated at the age of 15 in preparation for future implant placement. In addition, the upper third molars were transplanted to positions 35 and 45. After orthodontic treatment, a cone beam computerised tomography (CBCT) scan was taken for surgical treatment planning, including implant placement. Concave and knifed-edged bone in the upper jaw and the limited bone quality and quantity of the lower jaw indicated the need for bone augmentation. The materials selected were seven Astra EVä/® implants, and Bio-Ossä/® and Bio-Guideä/® for the hard tissue regeneration. Second-stage surgery for the low bone quality and hard tissue regeneration was scheduled for 6 months after placement. Two weeks after this minimally invasive surgery, prosthodontic therapy was initiated. Open-tray impressions were made to manufacture provisional, screw-retained crowns. The shape of the provisional restorations was adjusted by adding composite, putting pressure on the mucosa and optimising the pink aesthetics. Results: The treatment included orthodontic therapy, tooth transplantation, a fixed partial denture in the anterior mandible and seven single implants. Implant placement was via flap surgery and simultaneous guided bone regeneration (GBR) in the upper jaw. Reduced height, width and quality of alveolar bone are common in patients with congenitally missing teeth are; to deal with this, and to restore the buccal contour, GBR was deemed necessary. Implants were covered after 6 months and provisional restorations were made on teeth and implants. The patients is currently functioning with the provisional restorations, which have had a profound impact on his self-esteem. Permanent restorations will be placed after another 6 months. To date, the buccal contour of the implant sites has shown limited resorption. Conclusions: Treatment of oligodontia patients with dental implants is challenging because of the reduced height, width and quality of alveolar bone. This report demonstrated that a proper multidisciplinary treatment plan offers a predictable solution for complex cases. The choice of biomaterials significantly impacts on the final aesthetic outcome. -


IN VITRO AND IN VIVO CHARACTERISATION OF A NOVEL BONE-DEFECT-FILLING BMP-2-BIOCAP/HACC COMPLEX WITH SEQUENTIALLY ANTIBACTERIAL AND OSTEOINDUCTIVE PROPERTIES
Objectives: Bone grafts with both antibacterial and osteoinductive abilities are greatly needed for treatment of infected bone defects. In this study we developed such a bone graft with a sequential release system: burst release of the powerful antimicrobial agent, hydroxypropyltrimethylammonium chloride chitosan (HACC), followed by sustained release of the osteoinductive agent, BMP-2. Our hypothesis was that this would kill infection-associated bacteria and eventually induce osteogenesis to repair an infected bone defect. Methods: The minimum inhibitory concentration (MIC), minimum bactericidal concentration (MBC) and time–kill curve of HACC against methicillin-resistant Staphylococcus aureus (MRSA) were evaluated. The influence of HACC at concentrations of 1000, 200 or 40μg/mL on the proliferation of pre-osteoblasts was evaluated by measuring cell viability. The influence of 40μg/mL HACC on the BMP-2-induced differentiation of pre-osteoblasts was evaluated by assessing activity of alkaline phosphatase (ALP) , osteocalcin (OCN) expression and mineralisation. BMP-2 was first internally incorporated into biomimetic calcium phosphate granules to form BMP-2-BioCaP. HACC solution was then adsorbed onto its surface to obtain a BMP-2-BioCaP/HACC complex. Confocal laser scanning microscopy (CLSM) was used to observe the structure of BMP-2-BioCaP/HACC using FITC-BSA as a substitute for BMP-2 and staining HACC solution with rhodamine B. The release kinetics of FITC-BSA and rhodamine B were determined by quantitative spectrophotometric analysis. To evaluate osteoinductivity of the complex and to optimise the HACC concentration in vivo, the following groups (n=6) were randomly implanted into subcutaneous pockets in rats: (i) BMP-2-BioCaP/HACC complex (BMP-2-BioCaP/HACC-20, BMP-2-BioCaP/HACC-4 and BMP-2-BioCaP/HACC-0.8 according to content of 20, 4 or 0.8μg HACC); (ii) BMP-2-BioCaP; (iii)BioCaP/HACC; (iv) BioCaP. Five weeks after implantation, samples were retrieved for histological and histomorphometric analysis. Results: The MIC and MBC of HACC for MRSA were 40μg/mL. BioCaP/HACC completely eliminated MRSA within 24 hours. HACC at levels of 1000μg/mL and 200μg/mL (but not 40μg/mL) significantly suppressed cell viability. HACC at a level of 40μg/mL did not significantly influence BMP-2-induced ALP, OCN or mineralisation. Microscopy showed that BMP-2 homogenously distributed throughout BMP-2-BioCaP granules within BMP-2-BioCaP/HACC complex, forming a thin layer of HACC along the surface. The in vitro release profile showed rapid release of HACC, which was completely exhausted after 3 days; BMP-2 was gradually and slowly released, with only about 20% depletion after 30 days. Bone formation was observed only in the BMP-2-containing groups in the in vivo pro-fibrotic environment (subcutaneous sites). In comparison with the positive control group (BMP-2-BioCaP), BMP-2-BioCaP/HACC-4 and BMP-2-BioCaP/HACC-0.8 complexes resulted in similar levels of new bone formation, while BMP-2-BioCaP/HACC-20 was associated with significantly less new bone formation. Conclusions: BMP-2-BioCaP/HACC-4 complex can rapidly eliminate antibiotic-resistant bacteria and efficiently promote new bone formation both in vitro and in vivo – making this a promising material for repairing infected bone defects. HACC is a strong antibiotic that can be readily combined with other bone substitutes, such as Bio-OssTM/® to provide in situ antibacterial activity for bone regeneration associated with infection. -
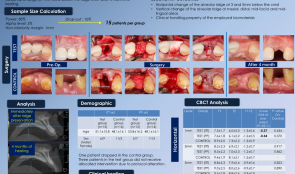

A RANDOMISED CLINICAL TRIAL FOR RIDGE PRESERVATION USING TWO TYPES OF COLLAGENATED XENOGRAFT/COLLAGEN MEMBRANE—A CONE-BEAM CT STUDY
Objectives: This randomised controlled clinical trial aimed to radiographically compare horizontal and vertical alteration of alveolar ridge following extraction-socket grafting with different combinations of biomaterials: collagenated porcine bone and cross-linked collagen membrane (test group) versus collagenated bovine bone and non-cross-linked collagen membrane (control group). Methods: This study included patients who required at least one anterior or premolar extraction, were aged 20 years old or more, and were able to understand the informed consent. Tooth replacement was planned using either conventional or implant-supported fixed partial dentures. Sample size calculations required 13 patients per group to obtain 80% power at a two-sided alpha level of 0.05%. A total of 30 patients were enrolled, and 15 were randomly allocated to each group. All were blinded to their allocations. Following a single tooth extraction, a collagenated bone substitute was used to fill in the socket, and a collagen membrane was used to cover it. Primary flap closure with several flap designs was attempted. Cone-beam CT (CBCT) scanning was carried out to assess the change in alveolar ridge, once immediately after ridge preservation and once after 4 months of healing. The primary outcome was horizontal alteration of alveolar ridge. Secondary outcomes were vertical alteration of alveolar ridge and clinical handling of the bone substitute and barrier membrane. Results: One patient in the control group dropped out and 3 patients did not receive the allocated intervention in the test group. Intention-to-treat (ITT; control group 14, test group 15) and per protocol (PP; control group 14, test group 12) analyses were performed. In the control and test group, 8 and 7 cases, respectively, showed membrane exposure, secondary healing was uneventful in all cases. There was no statistical difference in ITT and PP analysis between the groups in horizontal alteration of alveolar ridge width, but vertical height in the midfacial area was significantly reduced in the test group. The handling properties of the barrier membrane showed no statistically differences, but the handling properties of the bone substitute was significantly superior in the control group. Conclusions: Ridge preservation using collagenated porcine bone/cross-linked collagen membrane showed similar horizontal ridge alteration to collagenated bovine bone/non-cross-linked collagen membrane. However, vertical ridge changes were more pronounced with the collagenated porcine bone/cross-linked collagen membrane. Further studies including histometric evaluation are required. -


POLYSACCHARIDE NANOGEL CROSS-LINKED MEMBRANE FOR GUIDED BONE REGENERATION (GBR)
Takayuki Miyahara (Japan), Christer Dahlin, Anders Palmquist, Asako Shimoda, Myat Nyan, Yoshihide Hashimoto, Kazunari Akiyoshi, Shohei Kasugai Objectives: GBR is a bone augmentation technique that uses a barrier membrane to create a secluded space for unimpeded bone formation. In a previous report, a wet membrane of polysaccharide nanogel cross-linked (NanoClikä/®) hydrogel was successfully evaluated. The drawbacks of the material are shortshelf-life and difficulties in clinical handling. The purpose of this study was to evaluate the biological outcome of polysaccharide NanoClikä membrane for GBR. Methods: Bilateral symmetrical full-thickness parietal bone defects of 5-mm diameter were created using a bone trephine bur in 16 adult Wistar rats. Each defect was covered with a collagen membrane, a wet or dry NanoClikä membrane, or no membrane (control). The animals were sacrificed at 4 weeks and assessed using micro-CT and histology. Results: New bone formation in terms of bone volume in the bone defect was higher for both membrane groups compared to both control and collagen groups. There was no significant difference between the wet and dry membranes. Notably, the newly formed bone in the defect in both wet and dry groups was uniform and histologically indistinguishable from the original bone, but in the collagen group the new bone showed an irregular structure that was morphologically different from original bone. Conclusions: The dry NanoClik membrane stimulated bone regeneration to the same level as the wet membrane. -


VERTICAL RESORPTION OF AUGMENTED BONE AFTER SINUS LIFTING
Objectives: The use of a bovine-derived xenograft is a reliable alternative to autogenous bone when performing a sinus lift by means of the lateral window technique. Few studies report on the vertical resorption of the augmented bone, and these are mainly based on panoramic images. This retrospective case series aimed to assess vertical resorption of augmented bone by means of peri-apical radiographs. Methods: Between 2012 and 2013, patients underwent sinus lifting in two practices. Each augmentation procedure was performed using the lateral window technique and a bovine-derived xenograft (Bio-Ossä/®). Peri-apical radiographs were taken to assess the following parameters: initial native bone height (BH-B), bone height after sinus augmentation and implant placement (BH-IP), and bone height at tome of evaluation (BH-F). Results: Of a total of 70 eligible patients, 57 (mean age 56 years; SD11) could be evaluated. Mean follow-up time was 19 months (SD9). The parameters BH-B, BH-IP and BH-F were on average 3.87mm (SD1.74), 13.75 mm (SD2.12) and 13.11mm (SD 2.12), respectively. These differences were all highly significant (p Conclusions: Sinus lifting using the lateral window technique and bovine-derived xenografts is a predictable treatment. Irrespective of the initial native bone height, augmentation can be successfully achieved and only limited resorption is likely in the short term. -


SOFT-TISSUE VOLUME GAIN AROUND DENTAL IMPLANTS USING AUTOGENOUS SUBEPITHELIAL CONNECTIVE TISSUE GRAFT FROM THE PALATE OR TUBEROSITY—PRELIMINARY RESULTS OF A RANDOMISED PROSPECTIVE CLINICAL STUDY
Objectives: The main goal of this study was to compare the soft-tissue volume gain around dental implants with subepithelial connective tissue grafts (SCTG) originating from either palate or the tuberosity. The secondary goal was to compare changes in clinical parameters: plaque index (PI), bleeding on probing (BOP), probing depth (PD) and width of keratinised tissue (KT). Methods: Patients with single tooth implants already osseointegrated and in need of soft tissue augmentation were recruited (n = 12) and randomly received an SCTG from the palate (control group) or tuberosity (test group). Recipient sites were prepared by an intracrevicular incision at the buccal side extending to one adjacent tooth on each side, before raising a partial-thickness flap. Grafts of standarised dimensions were stabilised to the buccal flap and closure was achieved without tension. In order to examine volumetric tissue changes, an intraoral optical scanner was used to take two optical impressions at baseline and again 3 months after surgery. Digital software was used to superimpose the stereolithography (STL) files and calculate volume gain. Volumetric changes were calculated at three levels below the healing abutment on the buccal side of the implants (at 1.3mm and 5.0mm). The secondary outcomes were evaluated at baseline and at 3 months. Differences between control and teset groups were calculated for the quantitative variables using the Student’s t-test or Mann–Whitney test (depending on the normality of the distribution) and Chi-squared test for the qualitative variables. A p value of Results: No significant differences in baseline defect size were observed between groups. At 1mm volume gain was 1.28 ± 0.89mm for palate grafts (controls) and 1.28 ± 0.83mm for tuberosity grafts(p=0.39); at 3mm it wasoriginal, 84 ± 1.21mm for palate and 1.1 ± 0.4mm for tuberosity (p=0.31); and at 5mm it was 0.66 ± 0.23mm for palate and 0.95 ± 0.48mm for tuberosity (p=0.39). No statistically significant differences were observed at any level. The tuberosity grafts had a higher volume gain with a mean gain of 1.12 ± 0.57mm (versus a mean gain of 0.88 ± 0.94mm for palate), but these results were not statistically significant (p=0.42). Similarly, there was a tendency for higher KT gain for the tuberosity group, with an increase of 1.16 ± 0.98mm, versus 0.66 ± 0.82mm (p=0.36). A statistically significant reduction in PI was observed for the controls, from 18.0 ±0.89% to 16.3 ±1.03% (p=0.01), but only a slight (non-statistically) significant increase was seen in the test group. Non-statistically significant differences were also observed for PB and BOP. Conclusion: The main goal of this study was to compare the soft-tissue volume gain around dental implants using SCTGs of the same dimensions from either palate or tuberosity. Although the present data is only preliminary, procedures were effective in increasing volume gain around the implants at 3 months. Differences were statistically non-significant, but there was a tendency for increased volume gain with SCTGs from the tuberosity (1.12±0.57mm) compared to palate (0.88±0.94mm). Furthermore, there was a tendency towards for greater KT gain in the tuberosity group (1.16±0.98mm versus 0.66±0.82mm in the palate group). -


ANTIBODY-MEDIATED OSSEOUS REGENERATION (AMOR) IN THE RECONSTRUCTION OF ALVEOLAR RIDGE DEFECTS
Objectives: The aim of this study was to examine the efficacy of antibody-mediated osseous regeneration (AMOR) in conjunction with two novel extraction devices, namely a SocketKAP™ (for obturation of socket orifices) and SocketKAGE™ (for providing space in sites with facial dehiscence for ridge preservation and augmentation procedures following tooth extraction). Methods: In this prospective controlled study, 8–12-year-old macaques (Macaca fascicularis; n = 6) underwent removal of both maxillary and mandibular second left and right premolars (ULPM2, URPM2, LLPM2, LRPM2), both maxillary and mandibular second left and right molars (ULM2, URM2, LLM2, and LRM2) on each side. This was followed by resection of the entire facial alveolar wall. They were randomly assigned to the following intervention groups: dehiscence socket unfilled and uncovered (group A; negative control); dehiscence socket reconstructed with SocketKAGE™ and covered with SocketKAP™ (group B); dehiscence socket reconstructed with SocketKAGE™ and ABBM and covered with SocketKAP™(group C); dehiscence socket reconstructed with SocketKAGE™ and chimeric anti-BMP-2 monoclonal antibody (mAb) and covered with SocketKAP™(group D); dehiscence socket reconstructed with SocketKAGE™ and iso-type-matched control mAb (Iso-mAb) and covered with SocketKAP™ (group E). At 6 and 12 weeks post-extraction, cone beam CT imaging was performed. All files were imported to Simplant TM/® software (for linear measurement of remaining bone width and height at 1mm, 2mm, 3mm and 5mm from alveolar crest) and to reverse engineering Geomagic ControlTM/®software (for volumetric analysis of alveolar bone). Histologic evaluation was also made of the dimensional changes in dehiscence defects after ridge preservation using different materials. Non-parametric analysis of variance was conducted using the methods of Brunnner and Langer. Results: The result from linear and volumetric analyses demonstrated that group D (chimeric mAb +SocketKAP™ + SocketKAGE™) was associated with significantly greater percentages of remaining bone width and height at the buccal point, and remaining bone volume at 6 and 12 weeks when compared to group A (negative control), group B (SocketKAP™ + SocketKAGE™) and group E (Iso-mAb); the latter lost approximately 70% of crestal bone width at the crestal 1 mm point, and ABBM failed to prove more effective in preserving alveolar bone width at crestal 1mm (36%). When anti-BMP-2 mAB was used, the percentage of bone width was as good as those with ABBM at crestal 2mm, 3mm and 5mm areas. However, the most important finding was that the data demonstrated that bone remodelling using chimeric mAb was not only limited to the crestal 2–5-mm zone, but also the crestal 1-mm area, with mean remaining bone widths of 52% and 68% at 6 weeks and 12 weeks, respectively. Both CB-CT and volumetric analysis revealed more active and extensive bone regeneration of marginal bone with chimeric mAb compared to other groups. Histologic analysis showed the knife-edge of alveolar crest following tooth extraction in groups A, B, C and E, as well as statistically significant more bone remodelling in chimeric mAb, including a higher percentage of bone formation within newly generated tissue together with signs of osteogenic cell activity. Conclusions: These results suggest that chimeric anti-BMP-2 mAb, in conjunction with SocketKAPTM/® and SocketKAGETM/® was effective in the reconstruction of the alveolar bone in extraction sockets with facial dehiscence defects. These favourable results may be attributed to advantageous nature of AMOR, such as using endogenous BMP-2 captured by chimeric mAb enhance osteogenesis, with higher biological activity of endogenous BMP and a longer half-life of captured BMP compared to ABBM (which only exhibits osteoconductivity). -
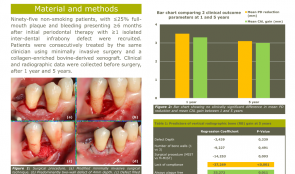

LONG-TERM OUTCOMES OF PERIODONTAL REGENERATION USING A COLLAGEN-ENRICHED, BOVINE-DERIVED XENOGRAFT IN A LARGE COHORT
Objectives: To evaluate the 5-year clinical outcome of regenerative periodontal therapy (RPT) using minimally invasive surgery and a collagen-enriched bovine-derived xenograft (1), and to identify predictors for gains in clinical attachment level (CAL) and vertical radiographic bone (RB) (2). Methods: Subjects were 95 non-smoking patients, with up to 25% full-mouth plaque and bleeding presenting at least 6 months after initial periodontal therapy with more than one isolated interdental infrabony defect. They were treated consecutively by the same clinician with combined surgery and xenograft. Clinical and radiographic data were collected before surgery, and after 1 year and 5 years. Results: Eighty-four patients (39 men, 45 women, mean age 53 years) were available for follow-up after 1 year and demonstrated a mean probing depth (PD) of 7.8mm, a CAL of 10.0mm and a defect depth of 5.2mm before surgery. Thirteen patients dropped out between year 1 and year 5. At 5 years, mean PD reduction was 3.3mm (SD 2.2 ), CAL gain was 3.0mm (SD 2.1) and RB gain was 57% (SD 38). Of these, 45% showed ≥4.0mm CAL gain, and 24% were considered failures (≤ 1.0mm CAL gain), 48% showed considerable RB gain (≥75%).The only predictor for CAL gain included sites that were always plaque-free during aftercare (p= 0.003). Predictors for RB gain included patient compliance (p=0.001) and sites that were always plaque-free during aftercare (p=0.010). Conclusions: Regenerative periodontal therapy using minimally invasive surgery and a collagen-enriched bovine-derived xenograft demonstrated favourable clinical and radiographic outcomes after 5 years. Oral hygiene and patient compliance had a significant impact in the long term. -


REHABILITATION OF A FIBULA-RECONSTRUCTED MANDIBLE BY USING COMPUTER ASSISTED IMPLANT SURGERY. A CASE REPORT.
Objectives: Reconstruction of mandibular integrity following a block resection is complicated by the loss of function and integrity of the graft. We report on rehabilitation of a patient who underwent mandibular resection and fibular reconstruction. Methods: A 16-year-old girl was referred to the Oral Implantology Department Clinic at the Istanbul University Faculty of Dentistry, 2 years after mandibular construction via a fibular graft. The geometry and topography of the graft was inconsistent and challenging for a removable prosthesis. To avoid the risk of fracture and necrosis, computer-assisted planning and flapless implant surgery was chosen as the best course of action. After obtaining a cone beam computerised tomography (CBCT) scan of the mandible with a radiographic template, the images were transferred into dedicated software and three implants were planned for shortened fixed composite–hybrid prostheses. Following surgery, one implant was found to be mispositioned and removed the following day. Results: The mandible was successfully restored by two implant-supported hybrid prostheses, fabricated with the use of nano-filled composite following the osseointegration period. Conclusions: Rehabilitation of a pathologically reconstructed edentulous jaw may be successfully completed using computer-assisted planning and guided implant surgery. Clinicians should be cautious regarding deviations related to the use of sterolithographic guides.









