-


FLAPLESS CRESTAL SINUS FLOOR ELEVATION USING PIEZOELECTRIC HYDRAULIC PRESSURE WITH IMMEDIATE IMPLANT PLACEMENT AND Bio-Oss COLLAGEN AS THE SOLE GRAFTING MATERIAL
Objectives: To reduce morbidity of lateral window sinus grafting using a minimally invasive (flapless) surgical technique with piezoelectric osteotomy and hydraulic pressure from the same instrument. The grafting material was Bio-Oss collagen, a well-documented material for regenerating bone in the maxillary sinus. Methods: Five patients in the private clinic of the author were randomly selected for the study, and cone-beam CTs (CBCTs) were taken. Patients with at least 3mm of bone from the crestal ridge to the floor of the sinus and a width of more than 6mm were recruited. In order to prevent resorption of the crestal bone, a flapless approach was used, with tissue punches. Preparation of the osteotomy and fracture of the floor of the sinus was performed using the Intra Lift Kitä/®. Hydraulic pressure was applied using the same instrument to lift the Schneiderian membrane. The integrity of the membrane was confirmed by the Valsalva test. Bio-Ossä/® collagen block was soaked in saline and cut in to pieces, then each piece was introduced into the osteotomy using tweezers and TKW5TM/®, beneath the elevated membrane. The diameter of all implants was 4.5mm. The osteotomy was undersized by about 1mm to ensure that all implants had good primary stability. They were covered with healing abutments on the day of surgery and IOPA were taken. After a 6-month‘ healing period, implants were progressively loaded with composite crown before final fabrication of the definitive crowns. Further CBCTs were taken after 6 months to confirm bone growth in the sinus. Results: Membrane perforation was observed in one patient in whom the implant was placed in the upper second molar region due to inadvertent slippage of TKW4TM/®. However no complications were reported. Newly formed bone along the implant was recorded in all cases, and average bone height gain was about 5mm. Conclusions: Although there was a perforation of the sinus membrane in one case, no complications occurred and there was bone gain and osseointegration of the implants. Given the small sample size of five cases, it seems that the minimally invasive approach using xenograft Bio-OssTM/® collagen as the sole grafting material, results in an average bone gain of 5mm and osseointegration of implants. -
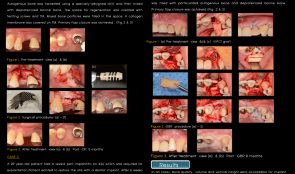

VERTICAL AND HORIZONTAL RIDGE AUGMENTATION USING TITANIUM MESH AND AUTOGENOUS BLOCK BONE
Objectives: Maintaining space is essential for predictable bone regeneration, especially in three-dimensionally collapsed defects. Titanium mesh (TM) and block bone grafting are known to have good space-maintaining capability. This report describes three cases of ridge reconstruction using TM and BG. Methods: Case 1 was a 45-year-old patient requiring the extraction of #25. Four months after extraction, guided bone regeneration (GBR) using TM was planned. Autogenous bone was harvested using a specially designed drill, and mixed with deproteinised bovine bone. The space for regeneration was created with tenting screws and TM. Mixed bone particles were used to fill the space, collagen membrane was covered by the TM, and primary flap closure was achieved. Case2 was 49 years old with severe peri-implantitis on #26, which was required for explantation. The patient wanted the site to be restored with a dental implant. Six weeks after explantation, free gingival graft was obtained for making a keratinised tissue zone. GBR using TM and tenting screws was scheduled for 4 months later. The surgical procedure was similar to that used in Case 1. Case 3 was 43-year-old patient with a periapical abscess on #22, the pathology of which affected the distal surface of the implant on #21. After extraction of #22, the severely damaged socket was treated with vascularised interpositional periosteal connective tissue graft. After 4 months, autogenous block bone was harvested, split in two sheets and fixed using screws buccally and palatally. The space created by the sheets was filled with particulated autogenous bone and deproteinised bovine bone before primary flap closure. Results: In all three cases, the quality, volume and vertical height the bone were acceptable. Conclusion: Ridge augmentation using titanium mesh combined with resorbable membrane or autogenous block bone is acceptable for implant placement. -


PLATELET RICH FIBRIN (PRF) WITH 0.05-MM THICK TITANIUM MEMBRANE FOR RIDGE AUGMENTATION OF SEVERE BONY DEFECTS IN THE AESTHETIC ZONE—A CASE STUDY
Objectives: Periodontitis and peri-implantitis may result in severe bony defects, which can be treated by titanium mesh. However, removal of the traditional 0.2-mm titanium mesh can be difficult. This report describes the use of a 0.05-mm thick titanium membrane (Ti-memb) in the aesthetic zone, with PRF in three patients with severe bony defects. Methods: Three patients presented for extraction in the aesthetic zone. Two months post-extraction, all three sites had severe deficiency in both vertical and horizontal dimensions. The sites were treatment planned for ridge augmentation with PRF and 0.05mm titanium membrane. Before surgery, 60mL of blood was obtained from each patient and PRF membranes were prepared according to the Choukroun method. A full-thickness flap was reflected to expose the vertical defect, and autogenous bone was harvested via decortication of the augmented site with a 5-mm diameter trephine inserted to a depth of 1–2mm through the cortical bone. The collected bone was mixed with DFBDA and soaked in growth factor-enriched PRF, before being placed in the augmentation site. Fixation screws were used to fixate the 0.05-mm titanium shield (10mm x 10mm) over the grafted site, in order to maintain the space needed. Two or three layers of PRF membrane were then placed over the titanium membrane in place of traditional resorbable membranes. Vestibular releasing incisions ensured passive tension-free flap closure, with 4-0 chromic gut sutures for vertical mattress fashioning for initial flap approximation and 6-0 polypropylene sutures for complete soft-tissue closure. Re-entry of the surgical site was performed after 6 months, for both implant placement and bone core biopsy for histomorphometric analyses. Cone-beam CT was carried out to visualise and quantify the bone augmentation. Results: All three surgical sites healed uneventfully. Clinically and tomographically, the titanium membranes maintained the space without signs of collapse. Upon re-entry, removal of the mesh was easily accomplished using a periosteal elevator. The underlying bone regeneration was robust in all cases. Clinically, there was a slight increase in keratinised tissue and no (or slight) change in vestibular depth. These soft tissue findings with PRF may arise because primary closure of flaps is not required. Histomorphometry indicated 47–56% new bone and 100% vital bone, and no fibrotic tissue or bacteria were observed. PRF allowed easy management of the soft tissue without using resorbable membrane. Conclusion: The use of PRF may promote soft tissue healing. Histomorphometry revealed favourable new bone and vital bone percentages compared to other bone regeneration protocols. The 0.05-mm titanium membrane showed excellent space maintenance as well as easy chairside modification and intraoral fixation due to its flexibility. The procedure was minimally invasive, easily to perform and cost-effective, thus PRF in conjunction with a 0.05-mm titanium membrane is an effective and simple treatment for severe bony defects that produces ideal sites for future implant placement. -


CLINICAL AND HISTOLOGIC EVALUATION OF A BOVINE-DERIVED XENOGRAFT (BDX) COMBINED WITH A NATIVE COLLAGEN MEMBRANE IN DEEP INTRABONY DEFECTS
Objectives: This study aimed to evaluate clinically and histologically the healing of deep intrabony defects after reconstructive surgery using a natural bovine xenograft (BDX) combined with a native collagen membrane (CM). Methods: Eight patients with severe chronic periodontitis and at least one tooth scheduled for extraction because of periodontal or prosthetic issues were included. Following local anaesthesia, full-thickness flaps were raised, and intrabony defects were exposed. Granulation tissue was removed from the defects and the roots were thoroughly scaled and root-planed by hand and ultrasonic instruments. A notch was placed in the root surface at the level of the calculus or the most apical point of the debrided root surface (if no calculus was present). Defects were filled with BDX (Cerabone[tm]) and covered with CM (Collprotect[tm]). Probing pocket depth (PD), clinical attachment level (CAL) and vertical probing bone level (PBL) were recoreded before and 9 months after reconstructive surgery. At 9 months, the teeth and surrounding soft and hard tissues were removed, fixed in buffered formalin and processed for histological analysis. Ground sections of 100µm thickness were cut and stained with toluidine blue and fuchsin and analysed under a light microscope. Results: All eight treated teeth presented deep (7.57 ± 1.16mm) one-wall intrabony defects. After 9 months, a reduction in PD (1.45 ± 1.35mm) and a gain in CAL (1.68 ± 0.62mm) was noted for all teeth. No adverse events related to the graft material or CM were observed in any biopsy tissue. Histology revealed the formation of cementum with inserting collagen fibers in the entire notch area in two cases, and new cementum at the apical extent of the notch in one case. Long junctional epithelium and biofilm formation were observed to varying extents in all cases; furthermore, graft particles were still present and encapsulated in connective tissue. There was some minute formation of bone in three biopsies, and three teeth showed signs of root resorption. Conclusion: In teeth with a poor prognosis, reconstructive surgery of intrabony defects using BDX and CM resulted in minimal or no periodontal regeneration. -

TECHNICAL NOTE ON THE MANAGEMENT OF POSTOPERATIVE INFECTIONS AFTER SINUS BONE GRAFTING—SINUS LIFT RESCUE
Objectives: Maxillary sinus bone grafting is now an integral part of dental implant procedures. Its main complication is postoperative infection in the grafted area. Removal of all graft material has been suggested as a way to manage this condition. This study involved a simple minimally invasive technique for managing local infections following sinus bone grafting, with the hope of avoiding graft removal. Methods: Between 2007 and 2015, more than 26 patients with sinus lift infections were treated using the following method. Two vertical 1-cm incisions were made on the vestibular area next to the infected area (to drain the postoperative maxillary sinus abscess), and a tunnel-like mucoperistal flap was elevated, and the collagen membrane used for covering the lateral bony wall was taken out. A Redon[tm] drain (Ch 6, DI 1cm, DA 2cm) was placed throughout the flap and secured with 3-0 silk sutures to both vertical incisions. The area was irrigated with 3% hydrogen peroxide solution two times each day for 10 days until no additional free-floating particles were observed. Patients were presecribed with amoxicillin clavulanic acid (1000mg three times per day), ibuprofen (600mg three times per day) and a special nasal spray (containing 1.14mg dexamethasone, 5mg naphazolin-HCl, 30mg chlorobutanol, 500mg popylene glycol, 3mg sodium monohydrogenphosphat, 50mg sodium dihydrogenphosphate aqua ad 10.0) twice daily for 10 days. Results: Twenty-six patients with sinus lift infections were treated. Ten days after drain insertion, the surgical area was free of symptoms. The drains were removed and vertical incisions were primarily closed. Implants were placed into the grafted areas 6 months later. Conclusion: Infection following sinus bone grafting is undesirable, whereby a second intervention may be needed requiring general anesthesia and/or a team approach, including an oral-maxillofacial surgeon and otolaryngologist. The simple and minimally invasive procedure described here may not offer a precise solution for infections associated with sinus bone grafting, but may be beneficial in terms of avoiding removal of bone graft material and preventing a more laborious procedure. Further clinical studies are needed to establish the success rate of the procedure. -
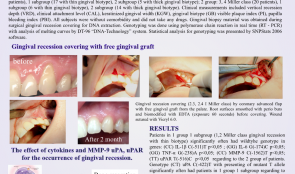

PREDICTIVE VALUE OF CYTOKINES (IL-1β, IL-6, TNF-α), MMP-9 AND uPA and uPAR GENE POLYMORPHISMS FOR CLINICAL OUTCOMES OF GINGIVAL RECESSION
Objectives: The objective of was to investigate the predictive value of single nucleotide polymorphism (SNP) in the promoter region of the cytokine interleukin(IL)-1β С(-511)Т; IL-6 G(-174)C; tumour necrosis factor(TNF)-α G(-238)A; matrix metalloproteinase(MMP)-9 С(-1562)T; urokinase plasminogen activator (uPA) С(-422)T; and urokinase plasminogen activator receptor (uPAR) T(-516)C gene as a risk modulator for the development of gingival recessions in adults. Methods: A total of 42 patients (age 270-35) with gingival recession were divided into groups: group I comprised 1, 2 Miller class (n = 22), with subgroup Ia (n = 17) with thin gingival biotype and Ib (n = 5) with thick gingival biotype; group II comprised 3, 4 Miller class (n = 20), with subgroups IIa (n = 6) with thin gingival biotype, and IIb (n = 14) with thick gingival biotype. Clinical measurements included vertical recession depth (VRD), clinical attachment level (CAL), keratinised gingival width (KGW), gingival biotype (GB), visible plaque index (PI) and papilla bleeding index (PBI). All subjects were without comorbidity and did not take any drugs. Gingival biopsy material was obtained during surgical gingival recession covering for DNA extraction. Genotyping was done using polymerase chain reaction in real time (RT-PCR) with analysis of melting curves by DT-96 DNA-Technology[tm] system. Statistical analysis for genotyping was presented by SNPStats[tm] 2006 software. Results: Patients in group Ia (1,2 Miller class recession with thin gingival biotype) expressed significantly more wildtype genotypes in genes (СС) IL-1β С(-511)Т (pwere not statistically significant. It was noticed that male patents aged under 40 [expressed?] high rates of mutant alleles in which genes for 1, 2 Miller class recession with thick biotype (group IIa). Conclusion: Carrying the mutant allele T gene uPA С(-422 )T in the promoter region appears to be a risk factor for developing gingival recession and is a potential predictor for more severe clinical phenotypes. -


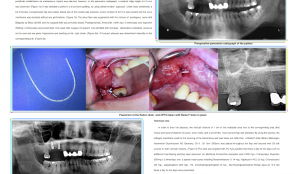
APPLICATION OF DENTAL IMPLANT TREATMENT FOR AESTHETIC AND FUNCTIONAL REHABILITATION OF ALVEOLAR CLEFT PATIENTS
Objectives: Patients with cleft lip and palate (CLP) frequently have a missing incisor at the alveolar cleft site. Owing to recent advances in secondary bone grafting (SBG) techniques, dental implant treatment has become an acceptable method for restoring the edentulous space at the cleft site in addition to conventional methods using bridges or dentures. In this study, we investigated the risk factors related to aesthetic outcomes of implant treatment at alveolar cleft sites. Methods: We examined a total of 13 patients (8 women, 5 men) treated with implants for missing teeth associated with an alveolar cleft at the Implant Clinic of the Dental Hospital at Tokyo Medical and Dental University between 2002 and 2010. The patients’ genders, cleft types and number of dental implants were recorded, as well as their ages at bone grafting for cleft closure, additional bone grafting prior to dental implant surgery, and dental implant placement. Three patients had a bilateral and ten had a unilateral cleft lip, alveolus and palate. Sixteen dental implants were evaluated. Risk factors such as lip line, length from the nasal floor to the alveolar ridge, width of the edentulous span, gingival margin of the adjacent teeth, and cleft types (bilateral or unilateral) were evaluated, and designated as either high risk or low risk. Results: Neither dental implant loss nor bone resorption around the dental implants were observed within 5 to 13 years after final restoration. All patients were satisfied with the aesthetic and functional outcomes, and all but one underwent bone grafting to close the alveolar cleft with autologous cancellous bone harvested from the iliac crest (SBG) between the ages of 11 and 28 years. Two underwent additional bone grafting before implant placement. The patients were 18–36 years old (mean 23) at the time of placement. In 11 patients, dental implants were installed at least 6 months after the last bone graft at the cleft sites. One patient did not undergo bone grafting before implant surgery, and one had an implant installed five months after the last bone grafting. Two cases with only low risk factors had good aesthetic outcomes of implant treatment. Out of the remainder, eight had one high-risk factor, one had three high-risk factors, and two cases had four high-risk factors at the time of placement. Aesthetic outcomes of the one high-risk factor group were slightly inferior to the no high-risk factor group, but they were still satisfactory. The value of aesthetic outcomes did not vary among the different types of risk factors; in contrast, aesthetic outcomes of the three and four high-risk factor groups were inferior to those of other groups. Conclusion: The time period between last bone graft at the cleft sites and placement of implants exceeded six months in most patients, but the grafted bone remained, and all implants were completely covered by host or grafted bone, with or without added bone substitutes or bone particles obtained during the drilling process for implant placement. Hydroxyapatite allografts were used in three patients, none of whom had signs or symptoms of infection or peri-implantitis at the grafted sites. Our results suggest that aesthetic outcomes may depend on the number of risk factors rather than the presence of high-risk factors. Two patients with no high-risk factors had a high-risk factor previously (width of the edentulous span), which was remedied by orthodontic treatment before implant surgery. Thus, it is important to reduce the number of high-risk factors to obtain good aesthetic outcomes from dental implant treatment for alveolar cleft patients. -


SINUS FLOOR AUGMENTATION AFTER ENDOSCOPIC SINUS SURGERY (ESS) FOR THE TREATMENT OF CHRONIC MAXILLARY SINUSITIS—A CASE SERIES
Objectives: The aim of this study was to evaluate maxillary sinus health in patients who underwent sinus floor augmentation for implant placement after endoscopic sinus surgery (ESS) for the treatment of chronic maxillary sinusitis. Methods: In this series, ESS was performed on four patients with chronic maxillary sinusitis before sinus floor augmentation. A two-stage sinus floor augmentation was performed using deproteinised bovine bone graft and non-cross-linked collagen membrane, 3 months later. Root-form dental implants were placed after 5 months of healing. Cone-beam CT (CBCT) images were taken before ESS, before and after sinus augmentation, and 3 years postoperatively. Sinus membrane thickness and ostium patency were evaluated during the observation period. Marginal bone loss for each dental implant was analysed by CBCT scanning and implant success was evaluated. All patients were rehabilitated with implant-supported fixed restorations. Results: All dental implants were placed in the grafted sinuses and the success rate was 100%. Sinusitis did not recur during the 3-year follow-up period. The ostiomeatal complex was not stenosed after ESS throughout the observation period, however the sinus membranes of two patients were thick and almost filled the sinus cavity before sinus floor augmentation. Corticosteroids were administered for 3 weeks to decrease the membrane thickness. Additive CBCT images confirmed membrane changes in these patients. On completion of medical therapy, sinus floor augmentations could be performed. Conclusion: ESS therapy before sinus augmentation is a reliable and predictable technique for achieving and maintaining the normal physiological environment of the maxillary sinus, after which dental implants can be safely placed in augmented sinus floor sites. CBCT scanning at regular intervals is recommended after ESS treatment for monitoring sinus membrane inflammation and ostium patency. -


EFFECT OF PERIODONTAL TREATMENT ON LEVELS OF PERIOSTIN IN GINGIVAL CREVICULAR FLUID (GCF) OF PATIENTS WITH CHRONIC PERIODONTITIS
Objectives: Periostin is an extracellular matrix protein that has a vital role in maintaining periodontal tissue integrity by forming a major part of the extracellular matrix (ECM). However, its role in vivo is yet to be elucidated. Hence this study was designed to assess the relationship between levels of periostin in the periodontium in healthy, diseased and healing humans. Methods: A total of 30 subjects were divided into two groups based on Russel’s Periodontal Disease Index (PDI) – healthy periodontium (group I; healthy) and chronic generalised periodontitis (group II; diseased). Gingival crevicular fluid (GCF) samples were collected using microcapillary pipettes from each participant at baseline, and at 2 weeks and 4 weeks after scaling root planing (SRP)in both groups, and at 2 weeks and 4 weeks after flap surgery in group II. Immunoblot assays were performed using a dot blot technique with appropriate antibodies. Spot densitometry analysis was performed with image analysis software. The correlation between periostin levels and various clinical parameters was analysed at baseline in both groups. Results: We found a mean level of periostin in the healthy group (I) as 423.6 ± 25.67, which was higher than that in the diseased group II (mean 148.07 ± 7.89). GCF levels of periostin correlated highly and positively (and statistically significantly) with PDI scores (p increased to 158.8 ± 10.93 at 2 weeks and to 170.2 ± 12.51 at 4 weeks post-SRP. These values further increased to 182.87 ± 12.41 at 2 weeks and 196.87 ± 19.01 ) at 4 weeks after flap surgery. All results were statistically significant (p Conclusion: These results confirm that periostin is highly expressed in healthy tissues and helps to maintain tissue homeostasis, and ;levels are downregulated during inflammation, as seen in the diseased group. Increasing levels of periostin after periodontal therapy indicate its role in wound healing. -


INVESTIGATION OF BISPHOSPHONATE-INDUCED TOXICITY ON DENTAL PULP STEM CELLS
Objectives: Osteonecrosis of the jaw is indicated by exposed alveolar bone and is associated with bisphosphonate therapy. This study investigated the cytotoxicity of two nitrogen-containing bisphosphonates, zoledronate (ZOL) and alendronate (ALN), on dental pulp cells (DPC) in vitro. Methods: DPC from third molar teeth were characterised by immunophenotyping and by differentiation into osteogenic and adipogenic cell lineages. The cytotoxicity of ZOL and ALN was assessed by MTT cell proliferation assay assay. Apoptotic events associated with DNA fragmentation were analysed using flow cytometry for the sub-G1 peak. Western blots were used to determine levels of the proteins Bax, Bcl-2 and caspase-3. Results: ZOL and ALN reduced cell viability in a concentration- and time-dependent manner. ZOL significantly decreased cell viability at a concentration of 100µm (p Conclusion: These findings extend previous observations that bisphosphonates at supra-physiological concentrations, in the absence of bone mineral, cause death of dental pulp cells.









