-


AESTHETIC TREATMENT OF PERI-IMPLANT SOFT TISSUE DEFECTS—A CASE REPORT OF A CORONALLY ADVANCED FLAP (CAF) WITH CONNECTIVE TISSUE GRAFT (CTG)
Objectives: Dental implant treatments at the anterior region of maxilla present challenges in terms of achieving a satisfactory aesthetic outcome. Peri-implant mucosal recession and gray titanium surface reflections may be may occur when soft-tissue thickness is insufficient. The case presented here involves using a coronally advanced flap (CAF) with connective tissue graft (CTG) to treat a peri-implant mucosal defect at a maxillary anterior single implant. Methods: A 33-year-old woman was referred because of the non-aesthetic appearance of her implant-supported crown in the maxillary lateral incisor. Intraoral examination revealed peri-implant mucosal recession and gray reflection with thin peri-implant mucosa. The CAF + CTG operation was planned to enhance soft tissue thickness and reduce recession height. CTG was obtained by means of disepithelisation of a free gingival graft, was harvested from the premolar region of palate and fully covered by coronally advanced flap. Results: Healing was issue free and sutures were removed after 10 days. The peri-implant mucosal recession was fully covered, the soft tissue was thickened, and there was no gray reflections at the peri-implant region. The peri-implant mucosa was stable when the patient was examined at 1 month, 3 months, 6 months and 12 months. Conclusion: CTG+CAF may be used to prevent implant surface transparency and to increase the peri-implant tissue thickness in aesthetic areas. -


CONNECTIVE TISSUE GRAFT (CTG) + PLATELET-RICH FIBRIN (PRF) COMBINED WITH GUIDED BONE REGENERATION (GBR) IN THE TREATMENT OF PERI-IMPLANT SOFT AND HARD TISSUE DEFECTS
Objectives: Hard and soft tissue deficiencies hamper the success of functional and aesthetic implant-supported restorations. There are many methods for peri-implant soft and hard tissue augmentation in aesthetic zone single-implants. This case report desxribes soft and hard tissue management of a patient using a connective tissue graft (CTG) + platelet-rich fibrin (PRF) combined with guided bone regeneration (GBR). Methods: A 30-year-old non-smoking woman with no systemic disease was referred to our clinic with dark reflection of an implant neck that had been placed 5 months previously in the lateral incisor area. Intraoral examination revealed a bone dehiscence defect in the vestibule of the implant body with thin peri-implant mucosa, and radiographic examination showed no bone resorption in proximal areas of the implant. After mucoperiosteal flap reflection, the dehiscence bone defect was augmented with xenograft and collagene membrane. To manage the peri-implant mucosa thickness, the CTG harvested from palate and the PRF membrane were placed over the collagen membrane. Results: The sutures were removed after 10 days and healing was uneventful. The thickness of the peri-implant mucosa was increased. The follow-up at 12 months showed that the mucosal thickness was maintained and the peri-implant mucosa was healthy. Conclusion: CTG+PRF combined with GBR resulted in the augmentation of soft and hard tissue in the peri-implant area with favourable aesthetic outcomes. -
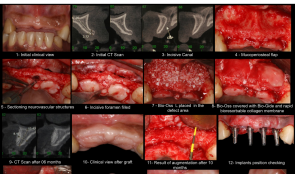

RIDGE AUGMENTATION BY APPLYING DEPROTEINISED BOVINE BONE MINERAL (DBBM) AND BIORESORBABLE MEMBRANE—A CASE REPORT
Objectives: Lateral ridge augmentations are traditionally performed using autogenous bone grafts, bone screws and titanium-reinforced ePTFE membrane; they are associated with considerable patient morbidity and a requirement for large flaps at second-stage surgery. The aim of this study was to determine whether the use of resorbable membranes and bone substitutes could lead to successful horizontal ridge augmentation, allowing the installation of implants in normal conditions, and thus minimising risks and morbidity to the patient. Methods: The patient presented with an anterior maxilla bone deficiency (canine–canine) preventing the placement of dental implants. The residual bone average was 2.5mm before bone augmentation surgery. Soft tissue flaps were carefully raised and particles of deproteinised bovine bone mineral (DBBM) (Bio-Oss[tm]) were placed in the defect area. A collagenous membrane (Bio-Gide[tm]) was applied to cover the DBBM and immobilised to the surrounding bone using only the soft tissue. The flaps were sutured to allow for healing by primary intention and to stabilise the DBBM and membrane. Results: Ten months after primary surgery, the average bone gain was 5mm and the bone crest was approximately 7mm after augmentation, allowing implant placement. When the flaps were raised for re-entry, the regenerated tissue appeared as mineralised bone tissue. Integration of deproteinised bovine bone particles into the newly formed bone was observed. Conclusion: Despite its limitations, this clinical case demonstrated that the combination of DBBM and collagen membrane may be used successfully for horizontal ridge augmentation. -


RETROSPECTIVE STUDY OF 147 IMPLANTS INSERTED IN AUGMENTED MAXILLARY SINUS AND 15-YEAR FOLLOW-UP OF MAXILLARY SINUS AUGMENTATION USING INORGANIC BOVINE BONE
Objectives: The study aimed to evaluate bone formation following maxillary sinus augmentation using bovine bone substitute material Bio-Oss[tm] and to determine the long-term success rate, using radiographic images of implants installed after sinus lifting procedure. Methods: Between January 2000 and October 2015, a total of 147 implants were placed in 64patients (24 men and 40 women), aged 34–87 years (meaan 57.39 years), in whom sinus lifting technique was performed on edentulous ridge bone (with 1–4mm residual bone height). Long-term evaluation involved comparing radiographic images at various time points from 99 cases of sinus floor elevation in the 64 patients, according to the technique described by Tatum (1986). Dental implants were inserted after 8 months of graft healing, and left submerged for 3 months. They were then loaded with provisional acrylic prostheses, which were replaced by definitive fixed metal–ceramic prostheses and followed for over 5 years of functional loading. All patients visited the clinic at 1 week, 2 months and 8 months in the first postoperative year, then at 1 year, 2 years, 5 years, 10 years and 15 years[ok?] thereafter, for clinical and radiographic examinations of the sinuses and implants, including CT imaging. Results: Twelve of the 147 implants were lost, giving a cumulative survival rate (CSR) of 91.83%. All lost implants were substituted and all patients who were followed had fixed prostheses functioning after 5 years of loading. Conclusion: This study suggests that the installation of implants after a sinus lift procedure combined with deproteinised bovine bone substitute material (Bio-Oss[tm]) graft in cases with pneumatisation of the posterior maxilla have predictable high survival rates. The procedure is a reliable option for the placement of implant-supported prostheses in patients with increased pneumatisation of the maxillary sinus and atrophic alveolar bone. -


MORPHOLOGICAL EVALUATION OF SOFT TISSUE AUGMENTATION USING POROUS POLY-D, L-LACTIC ACID WITH STRAIGHT HOLES
Objectives: This study aimed to investigate the biological reaction to porous poly-d, l-lactic acid (PDLLA) scaffolds with holes for soft tissue augmentation. Methods: The control group consisted of porous PDLLA with a diameter of 5.0mm and a height of 2.0mm. For the two test groups, seven holes were drilled in the topof the scaffolds, with a diameter of 0.5mm and height 1.0mm. Each scaffold was placed in the periosteum of cranium and their height and molecular weight was measured at 4 and 8 weeks. Frozen sections were prepared from one sample from each group, to allow observation of the relationship between the material and cells. Paraffin-embedded sections were stained with haematoxylin and eosin to measure the areas of connective tissue and blood vessels. Results: The scaffolds from all groups had similar heights at 4 and 8 weeks, but their molecular weights decreased significantly over time. Significant differences were observed in connective tissue and blood vessel areas among the control scaffold no holes, and scaffolds with 0.5-mm and 1.0-mm diameter hole at both time points. Direct connection was observed between the material and cells. Conclusion: The amount of soft tissue increased with PDLLA drilled with straight holes. The straight holes kept the area of connective tissue. Neither molecular weight nor height of the scaffold were affected by the existence or size of the holes, but the area of connective tissue and blood vessels increased significantly in PDLLA containing holes, whereby holes of larger diameter showed greater areas. -
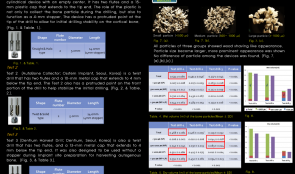

VOLUMETRIC COMPARISON OF THREE DIFFERENT INNOVATIVE BONE-COLLECTING DEVICES FOR AUTOGENOUS BONE GRAFTS
Objectives: The aim of this study was to clinically evaluate three different bone-collecting devices throughvolumetric analysis. Methods: Bone particles were harvested from bovine mandibles using three different collecting devices (1, 2 and 3) and ten drilling sites in each group. Bone particles were then filtered through sieves with openings of 500μm and 1000μm and divided into three groups according to size: 1000μm (large; LP). Total wet volume, fractional wet volume, fractional dry volume and weight were recorded and the shapes of the dried particles were examined using a microscope. Results: The bone particles in all three groups had the appearance of wood shavings. Collecting devices 1 and 2 primarily yielded LPs (0.510±0.064 mL, 0.430±0.067 mL, respectively). For device 3, MPs were most common (0.112±0.019 mL). The wet volume of both SPs and MPs obtained using device 3 was significantly greater than from devices 1 and 2 (p Conclusion: The three innovative bone collecting devices studied here collected comparable amounts of bone particles for potential use in commercial bone graft materials. -


BEHAVIOR AND DIFFERENTIATION OF OSTEOBLASTS ON A TITANIUM SURFACE WITH DIFFERENT MICROMETRE-SCALE ROUGHNESS
Objectives: Titanium implants with mean arithmetic roughnesses (Ra) of 1–2µm are associated with improved osseointegration and clinical outcome. However, the procedures used for producing a roughened surface usually change other parameters, such as spatial characteristic skewness and kurtosis, and sub-micrometre and nanoscale roughness. Studies are needed to explore the effect of different surface characteristics on osseointegration and clarify the relationship between Ra and osseointegration. This study aimed to investigate how titanium surfaces with different micrometer-scale roughnesses influenced proliferation, migration and differentiation of osteoblasts in vitro. Methods: Titanium replicas with surface roughnesses (Ra) of approximately 0µm, 1µm, 2µm and 4µm were produced. The surfaces have no significant sub-micrometre or nanoscale roughness and have similar skewness and kurtosis. MG-63 osteoblasts were cultured on the surfaces for up to 5 days and their behavior was investigated using time-lapse microscopy. The speed of cell migration was quantified using specialised software. Gene and protein expression were determined for alkaline phosphatase (ALP), osteocalcin and vascular-endothelial growth factor (VEGF). Results: Cell migration speeds were significantly lower on surfaces with Ra of about 4µm compared to those with lower Ra levels, with no differences between those with Ra in the range 0–2µm. Cell proliferation decreased gradually with increasing Ra. Gene expression of ALP, osteocalcin and VEGF was greater for the 1-µm and 2-µm Ra surfaces than the 0-µm and 4-µm surfaces. These findings were similar for protein expression. ALP and osteocalcin content in the conditioned media were significantly higher for cells grown on the 2-µm Ra surface compared to the 0-µm and 4-µm surfaces. The production of VEGF by cells on the 1-µm and 2-µm surfaces was significantly higher than that of the 0-µm surface. Cells grown on the 2-µm surface produced significantly more VEGF than those on the 4-µm surface. Conclusion: Surfaces with lower and higher roughnesses in this study seem to be suboptimal for osteoblasts. We suggest that decreased cell migration on surfaces with Ra 4µm might be associated with decreased osteoblast differentiation, probably through inhibition of cell-to-cell contact. -


EFFECT OF VITAMIN D-LOADED BONE SUBSTITUTES ON OSTEBLASTOGENESIS AND OSTEOCLASTOGENESIS IN VITRO
Objectives: Vitamin D deficiency is common, especially in elderly people, but elevating systemic levels through supplementation before surgery requires extensive effort. Local application of vitaminD-loaded bone substitutes is one alternative. However, the optimum carrier material is unknown. We assessed the effect of vitamin 25(OH)2 D3 and 1,25(OH)2 D3 (vitamin 25D, 1,25D)-loaded deproteinised bovine bone mineral (DBBM) on its own or with collagen (DBBM/C) on the genesis of osteblasts and osteoclasts. Methods: DBBM and DBBM/C were loaded with vitamin 25D and 1,25D and lyophilised. Surface structure loaded and unloaded materials was assessed using scanning electron microscopy (SEM). Release kinetics were assessed using supernatants generated after 1, 3, 6, 24 and 48 hours, and the effect of the supernatants on osteoblastogenesis and osteoclastogenesis was evaluated. MC3T3-E1-based alkaline phosphatase (ALP) was used for osteoblastogenesis; for osteoclastogenesis, RAW 264.7 cells were used in the presence of receptor activator of NF-κB ligand (RANKL) based on the numbers of multinuclear tartrate-resistant acid phosphatase (TRAP)-positive cells. MTT tests were also used to assess viability of MC3T3-E1 and RAW 264.7 cells. Results: The SEM images show no changes in the surface structure of loaded bone substitutes after loading with vitamin 25D and 1,25D. The osteoblastogenesis assays showed that supernatants of DBBM/C reduced ALP levels for up to 6 hours regardless of the type of vitamin D, while no substantial effects were observed with supernatants of DBBM alone. These findings paralleled the reduction in formazan formation in the presence of supernatants from DBBM/C taken in the first 6 hours. The osteoclastogenesis assays revealed a strong reduction in the number of TRAP-positive multinucleated cells in RAW 264.7 cultures when treated with supernatants of DBBM/C, while no substantial effects of supernatants of DBBM were observed. Overall the reduction in osteoclastogenesis was more pronounced than the reduction in osteoblastogenesis. Conclusion: Our findings suggest that regardless of the type of vitamin D used, DBBM/C has a stronger paracrine-like activity than DBBM, leading to a reduction of osteoblastogenesis and osteoclastogenesis. Overall, the inhibition of osteoclastogenesis was more pronounced, suggesting an antiresorptive effect, thus it is important to consider these properties when using bone substitute materials as carriers for vitamin D. -


IMMEDIATE LOADING IN POST-EXTRACTION SITES WITH MACHINE SURFACE IMPLANTS—A REPORT OF 63 CASES
Objectives:A recent, significant breakthrough in oral implantology was immediate implantation following tooth extraction, which reduces the number of surgical procedures required. The aim of this study was to test whether or not machine-surfaced implants, used for immediate loading of single-implant crowns in post-extraction sites, yields different results from conventional submerged two-stage implant positioning in healed sites with rough implants, in terms of implant survival after 6 months. Methods: Patients over 18 years of age requiring a single immediate post-extraction implant in the aesthetic area were enrolled in the study. The two adjacent teeth were required to be present. After gentle tooth extraction, a machine-surfaced implant (iMAXpro[TM]) with internal hexagonal connection was used. Different implant lengths and diameters were selected depending on the patient’s anatomy. Each implant was immediately loaded with a screw-retained provisional restoration. Implant insertion torque was also assessed with a manual wrench and reported as > 35 N/cm. The extraction socket had at least three intact walls, with partial dehiscence allowable on the fourth wall. If there was a residual gap of > 1mm between the implant surface and the buccal bone wall, it was filled with bone substitute (BioOss[tm] deproteinised bovine bone granules). After 6 months of follow-up, final prosthetic restoration was performed. Results: A total of 63 immediate loading post-extraction implants were positioned. All implants had uneventful healing, but five failed within 6 months. The implant success rate at 6 months was 92%. According to a defined standard, 58 implants fulfilled all the criteria of implant success: absence of persistent subjective complaints, such as pain, foreign body sensation, and/or dysaesthesia; absence of a recurrent peri-implant infection with bleeding and/or suppuration; absence of mobility; and absence of continuous radiolucency around the implant. No patients needed any additional surgical or pharmacological therapy. No implants showed signs of damage, such as fracture or bending. In 55 cases, the gap between the implant surface and buccal bone wall was > 1mm and was filled with BioOss[tm] granules, and in all cases there was a wound healing without complication, comparable to cases with no graft. Conclusion: Immediate implant placement with immediate loading provides good treatment outcomes and allows good functional and aesthetic results. It also addresses the psychosocial aspects of dental extraction. However, to achieve satisfactory results it is necessary to carefully select clinical cases and strictly apply the surgical and prosthetic protocols, with a well-trained team capable of controlling the surgical and prosthetic problems that can arise. In this study, the machine-surfaced fixture was shown to be effective for immediate loading of post-extraction implants, but it is necessary to follow-up all implants for a longer period. All patients will be checked again at 1, 2, 3, 4 and 5 years after implantation, using intraoral radiographs and aesthetic evaluation to confirm whether outcomes are comparable with conventional two-stage surgical techniques and other implant surfaces. -


PERIODONTAL REGENERATION VIA CELL HOMING
Objectives: The innate healing potential of periodontium has emerged as a new focus for regenerative therapies. Consequently, cell homing is appealing because it relies on attraction of the patient’s own stem cells. Stromal cell-derived factor-1 alpha (SDF-1α) plays a major role in this process. The aim of this study was to develop a construct for periodontal regeneration based on cell homing with SDF-1α, and to evaluate its effect on early and late wound healing in a periodontal defect model. Methods: For the preparation of the construct, gelatin sponge loaded with recombinant human SDF-1α was used. The release kinetics of SDF-1α were studied in vitro. A transwell migration model was used to test the in vitro homing capability of the SDF-1α construct for rat bone marrow stromal cells (BMSCs). Subsequently, constructs were tested for efficacy in a validated rat periodontal model. In 48 athymic nude rats, intrabony periodontal defects were created unilaterally and implanted with either (i) SDF-1α-loaded gelatin sponge, (ii) gelatin sponge, or (iii) left empty as a control for evaluation periods of 1 and 6 weeks (n=8). Evaluation consisted of descriptive histology, histomorphometry (epithelial downgrowth, inflammation, functional ligament length, new bone area, new bone height) and micro-CT (volume newly formed bone). In vivo recruitment of rat BMSCs to the defect site was tested immunohistochemically, whereby green fluorescent protein (GFP)-transgenic rat BMSCs were injected into the tail vein of the rats. GFP-positive cells in the defect site were quantified in situ by flow cytometry in 12 nude athymic rats using the same experimental set-up. All measurements were subjected to statistical analysis with ANOVA and differences were considered significant at p Results: The in vitro release experiment showed limited release of SDF-1α (picogram quantities following nanogram loading). The transwell migration model proved the site-homing capability of the SDF-1α construct in vitro for the rat BMSCs. At 1 week post-implantation, the histological tissue response in the defect was similar for all groups, with epithelial downgrowth, inflammation (30%), minor bone formation and no periodontal ligament formation. At 6 weeks post-implantation, SDF-1α constructs showed more newly formed bone area and height (0.4mm versus 0.2mm and 0.13mm versus 0.8mm), longer relative functional ligament (0.3mm versus 0.2mm) and less inflammation (6% versus 12%) compared to gelatin controls. However, the differences between the SDF-1α group and empty defects were not significant, except for newly formed bone height (14% versus 7%). Epithelial downgrowth was comparable for all groups at 1 and 6 weeks. The micro-CT data supported the histomorphometrical findings. The volume of the newly formed bone for SDF-1α constructs was significantly higher than for both gelatin and empty controls after 6 weeks (18% versus 10% and 8%). At 1 and 6 weeks post-implantation, no GFP-positive BMSCs were detected in the defect. Conclusion: The SDF-1α construct significantly improved periodontal wound healing at 6 weeks in terms of bone regeneration. In view of suboptimal release kinetics of SDF-1α from the gelatin sponge, alternative carriers need to be explored to maximise the potential for bone regenerative procedures via cell homing.









