-


EFFECTS OF PLATELET-RICH PLASMA (PRP) PRODUCTS ON VIABILITY AND PROLIFERATION RATE OF HUMAN GINGIVAL FIBROBLASTS (HGF)
Objectives: Platelet preparations are increasingly used to improve bone and soft tissue regeneration, but basic studies are insufficient for supporting the real efficacies of these products. Controversy exists about the effects of platelet product on hard and soft tissue regeneration, therefore more in vitro studies are needed. The aim of this investigation was to compare the in vitro effects of platelet-rich growth factor (PRGF) and platelet-rich fibrin (PRF) on the proliferation of human gingival fibroblasts (HGF). Methods: Whole blood samples were collected from a healthy volunteer. Anitua's PRGF and Choukran's PRF were prepared according to standard protocols. After culture periods of 24, 48 and 72 hours, HGF cell proliferation was evaluated by MTT assay. Statistical analysis was performed using one-way ANOVA followed by Tukey-Kramer’s multiple comparisons and p values less than 0.001 were considered significant. Results: The optical density of the negative control (fetal bovine serum (FBS) 1%) was set at 100% and other groups were expressed as a percentage of this. Our results showed PRGF treatment induced statistically significant (p 1.73%, p Conclusion: PRGF has a strong stimulant effect on HGF cell viability and proliferation compared to PRF. Further comparative studies of PRF and PRGF are needed using more cell lines and primary cells with different in vitro proliferation assays and more in vivo assays. -


THE EFFECT OF FIBRIN-BINDING OLIGOPEPTIDE DERIVED FROM FIBRONECTIN ON MIGRATION OF PERIODONTAL LIGAMENT CELLS IN AN IN VITRO WOUND HEALING MODEL
Objectives: The aim of this study was to evaluate the effect of synthetic FN fragments containing an N-terminal fibrin-binding domain on migration of human PDL fibroblast cells in an in vitro wound-healing model. Methods: Three types of synthetic oligopeptides (FF1, FF3 and FF5; including fibrin-binding domain FN) were allocated to the experimental groups. Recombinant oligopeptide (F20) including type Ш 9–10 domains of FN was as a positive control, and a group treated with nothing was the negative control. Cell migration capacity was evaluated using an Cell Migration Assembly kit. Results: The migration rates and number of migrated cells increased in the test group and both control groups at each point in time (6, 12, 18 and 24 hours). The F20 (positive control) group showed a significantly greater cell migration rate than the control group at 6 and 12 hours (but not at 18 or 24 hours). There were no significant differences among the test groups or between the test and positive control groups (F20) (p Conclusion: Within the limits of this study, the N-terminal fibrin-binding domain of FN was observed to promote cell migration of PDL fibroblast cells. -


BONE-REGENERATIVE ACTIVITY OF PARATHYROID HORMONE (PTH)-RELEASING NANO-HYDROXYAPATITE/POLY(L)-LACTIC ACID (PLLA) HYBRID SCAFFOLDS
Objectives: The study aimed to fabricate a novel bone-regenerative scaffold based on systematic combination of porous organic–inorganic hybrid scaffolds and recombinant human parathyroid hormone (rhPTH). Methods: The hybrid scaffold was fabricatedby immobilisation of polyphosphate-functionalised nano-hydroxyapatite (PP-n-HAp) on the surface of porous poly(l)-lactic acid (PLLA) scaffolds. This was followed by rhPTH loading on the polyphosphates of n-HAp surfaces. The surface polyphosphate functionalities of PP-n-HAp enabled stable chemical immobilisation of n-Hap on the amine-treated pore surface of the PLGA scaffolds. RhPTH with a positive charge was bound at a high efficiency of 98.1–99.5% onto the anionic polyphosphates of PP-n-HAp immobilised on PLLA surfaces and was released sustainably for up to 50 days. The release rate was manipulated by adjusting the amount of loaded rhPTH, and the release data were moderately fitted to the Higuchi’s diffusion model. Results: Immobilisation of PP-n-Hap was performed with a 1-ethyl-3-(3-(dimethylamino)propyl)carbodiimide (EDC)-mediated coupling reaction between the acidic PP groups and the primary amine groups on the surface of amine-functionalised PLLA scaffolds. They have a mean surface pore size of 110±10μm. Even after PP-n-HAp immobilisation, the initial interconnected pore structure and pore diameter were maintained. The pore size of PP-n-HAp-PLLA scaffolds may allow the spaces enough forthe growth of bone-forming cells. Thermogravimetric analysis (TGA) showed that the amount of immobilised n-HAp on the pore surface of PLLA scaffolds was 11.3 wt%. The dose-dependent sustained release patterns of rhPTH from PP-n-HAp-PLLA scaffolds were confirmed by a release profile. Four types of scaffolds were tested in rabbit calvaria defect models: (i) PLLA only, (ii) PP-n-HAp-PLLA, (iii) rhPTH (2mg) loaded PP-n-HAp-PLLA, and (iv) rhPTH (10mg) loaded PPn-HAp-PLLA. After 5 weeks, rhPTH-loaded PP-n-HAp-PLLA (with 2mg and 10mg rhPTH) displayed higher bone growth than the control group (PLLA only). Conclusion: We described the fabrication of porous PLLA scaffolds with rhPTH-releasing PP-n-HAp for bone regeneration. This hybrid scaffold was prepared by PP-n-HAp immobilisation onto the PLLA scaffolds, followed by the sequential rhPTH loading on PP-n-HAp. RhPTH was incorporated with high efficiency, and the sustained release of rhPTH from the hybrid scaffolds was observed for up to 50 days. In the animal experiment, we showed that the pore surface of the PLLA scaffolds had a synergistic bone-forming effect, not only due to surface-exposed osteoconductive n-HAp but also due to the sustained release of rhPTH. This bone-regenerative hybrid scaffold may find broad applications as a bone generation material. -


BONE GROWTH ON TITANIUM IMPLANTS AFTER ELECTRICAL STIMULATION
Objectives: The aim of this study was to measure the contact area of the bone–implant interface on implants submitted to different electric currents. Acceleration of healing time by electric stimulation in animals is still controversial, although several authors have demonstrated that electricity can stimulate bone formation around dental implants, depending on the intensity and period of the impulse as well as the treatment period. Methods: Ninety titanium dental implants measuring 6 mm x 11.5mm and with machined surfaces were used study. They were sterilised using gamma rays. Six male Beagle dogs approximately 12 months old and weighing 15kg were divided randomly into two groups for evaluation at 7 days and 15 days (three animals each time). Three levels of electrical stimulation were delivered to the implants (10μA, 20μA; control 0μA) through an electrical device coupled to the implant connection area. Results: No statistical differences was found in the contact area at the bone–implant interface after for 7 days of electrical stimulation. However, a significant higher contact area was recorded for stimulation at 20μA compared to 10μA and controls (p 0.05). Conclusion: The electrical stimulation of dental implants can increase the contact area at the bone–implant interface due to bone formation. The effect of different electrical current intensities and periods should be studied further to clarify the potential of this method. -


AZITHROMYCIN-RELEASING POLYMERIC MEMBRANES FOR GUIDED BONE REGENERATION (GBR)
Objectives: The objective of this study was to develop and evaluate a calcium phosphate-coated polycaprolactone (PCL) electrospun membrane loaded with azithromycin, in order to make use of the antimicrobial and anti-inflammatory properties of the antibiotic in GBR. Methods: PCL membranes were fabricated via solution electrospinning. Azithromycin at three different doses (1mg, 2.5mg and 5mg) was dissolved in ethanol (100%) and loaded onto the PCL- and calcium phosphate (CaP)-coated membranes. The membrane discs were soaked in the antibiotic solution for 8 hours befor evaporating off the solvent at room temperature. The release profile at different azithromycin concentrations was evaluated by colorimetric assay. Membrane surface morphology was assessed using scanning electron microscopy, surface area analysis for surface area and porosity, and electrokinetic analysis for surface charge. Chemical composition was determined by X-ray diffraction. Antimicrobial activity in vitro was determined by disk diffusion for up to 14 days. In vivo analysis was carried out by applying the membranes to critical size calvarial defects (5mm diameter) in Sprague Dawley rats. Bone formation was assessed by micro-CT, histology and histomorphometry. Results: Azithromycin was successfully loaded onto PCL/PCL-CaP membranes with a high loading efficiency of up to 85%. The release profile showed rapid release of the drug within the first 24 hours, followed by linear release over the next 14 days. The release profile was similar for all doses, but the amount released in both initial and late stages was significantly affected by the initial dose: for the 1-mg dose, 80% of the drug was released at 24 hours, with total release after 14 days; the higher doses (2.5mg and 5mg) showed 20% and 50% release at 24 hours and 14 days respectively. This controlled and sustained release of azithromycin was able to inhibit bacterial growth in vitro for up to 14 days. Application of azithromycin-loaded PCL-CaP membranes in rat calvarial defects demonstrated improved bone regeneration after 8 weeks of implantation for antibiotic-loaded membranes compared to unloaded controls. Conclusion: Hydrophobic azithromycin was successfully encapsulated on to PCL/PCL-CaP membranes using an ethanol evaporation technique. Excellent encapsulation efficiency was observed, along with a controlled-release profile and efficient antibacterial properties. The azithromycin-loaded membranes showed enhanced bone formation compared to unloaded controls. These results suggest that azithropmycin-loaded membranes have both osteogenic and antimicrobial properties that may be clinically useful for enhancing GBR procedures. -


THE USE OF BIOACTIVE GLASS AS BONE SUBSTITUTE IN ORAL IMPLANTOLOGY—A CASE SERIES
Objectives: The aim was to present our patient experiences and clinical outcomes following the use of bioactive glass bone graft material (Leonardo[tm]) in various dental implant procedures. Methods: The procedures included alveolar ridge splitting, immediate implant placement, sinus lifting, cyst removal and bone grafting followed by implant placement and management of a bone defect around the implant in the aesthetic zone. Results: All patients tolerated these procedures well and had no postoperative complications. The clinical and radiological results were satisfactory. Conclusion: Despite the limitations of this case series, synthetic bioactive glass is a promising material for improving therapeutic outcomes in dental implantology. -
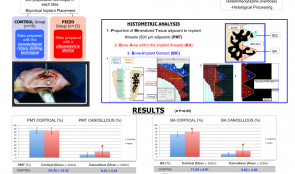

THE INFLUENCE OF PIEZOSURGERY ON BONE HEALING AROUND TITANIUM IMPLANTS – A HISTOLOGICAL STUDY IN RATS
Marcelo Sirolli(Brazil), Carlos Eduardo Secco Mafra, Rodrigo Albuquerque Basílio dos Santos, Luciana Saraiva, Marinella Holzhausen, João Batista César Neto Objectives: The aim of this study was to investigate the influence of two techniques for dental implant site preparation on bone healing around titanium implants. Methods: Fifteen male Wistar rats (weighing approximately 300g) were used. Tibias were randomly assigned to undergo implant site preparation with a conventional drilling technique (control group) or piezoelectric device (piezo group). After 30 days, they were sacrificed and the following histomorphometric parameters were evaluated separately for cortical and cancellous tibial regions: proportion of mineralised tissue (PMT) adjacent to implant threads (500μm adjacent); bone area within the threads (BA); and bone–implant contact (BIC). Results: There were no differences between the two groups for cancellous BIC (p>0.05) and cortical PMT (p>0.05). A higher mean percentage of BA was observed in the piezo group in cortical regions (controls 71.50% ± 6.91 and piezo group 78.28% ± 4.38; pin cancellous regions (controls 9.35% ± 5.54 and piezo 18.72% ± 13.21; p Conclusion: Within the limits this study on implant site preparation, we conclude that piezosurgery favours bone healing rates in cancellous bone regions, while the drill technique gives better results in cortical regions. -


126 ANTERIOR DENTAL ROOT FRACTURES—PRESERVATION OF THE ALVEOLAR RIDGE USING IMMEDIATE IMPLANT PLACEMENT
Objectives: The aim of this study was to evaluate clinical treatment of immediate dental implant placement of root fractures in adult patients following dentoalveolar trauma. Methods: A descriptive study was performed for cases of root fractures by systematic review of the digital records of all patients with dentoalveolar trauma and root fractures between May 2009 and May 2010 at the Unit of Oral and Maxillofacial Surgery, Hospital Clínico Mutual de Seguridad C.Ch.C., Santiago de Chile. Results: A total of 894 dentoalveolar trauma cases were identified, of which 56 (6.3%) were root fractures. In terms of outcome, implants had a 98% success rate, with no complications associated with vestibular bone loss or gingival unaesthetic recession. Conclusion: We believe that immediate replacement of lost teeth after root fractures with dental implants is a reliable option for patients with dental trauma, with no vestibular bone loss complications in the short term. -


THE FATE OF BUCCAL BONE AROUND DENTAL IMPLANTS—A 12-MONTH POST-LOADING FOLLOW-UP STUDY
Objectives: Buccal bone thickness is considered to be an important factor during implant surgery. Its resorption might have an effect on soft tissue stability and eventually on implant survival. This study aimed to investigate the resorption of buccal bone during the first 12 months after implant loading. Methods: The study included 24 patients (47 implants). Buccal bone thickness was measured during implant surgery at several distances from the implant shoulder using a specifically designed device that allows bone thickness measurements without requiring elevation of a mucoperiostal flap. The measurements were repeated after 12 months of loading. Sixteen implants were placed flapless and 31 with the elevation of a flap. Of the latter, 19 were placed following a one stage protocol and 12 following a two-stage protocol. Results: The mean reductions in buccal bone thickness, when all groups were pooled, were 0.26mm,0.36mm,0.35mm and 0.27mm at the shoulder, and 2mm, 4mm and 6mm apically. Implants with initial bone thickness of Conclusion: Various authors have claimed that an initial buccal bone thickness of 2mm is necessary for preservation of the buccal bone plate. It was hypothesised that thin buccal plates are less resistant to different types of trauma that implants can endure and are therefore more prone to resorption and buccal implant exposition. Within the limitations of this study, one might question the necessity of having a thick bone plate at the vestibular site of the implant. -
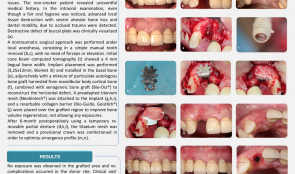

GUIDED BONE REGENERATION (GBR) IN THE AESTHETIC ZONE—RESTORATION OF HORIZONTAL BONE DEFECTS WITH MIXED BONE GRAFT AND TITANIUM MESH
Objectives: To report a case of a severe horizontal defect in a maxillary lateral incisor in which GBR was applied with adjunctive use of autologous (mandibular body cortical) bone and xenogeneic bone graft (BioOss[TM]), combined with titanium mesh, to improve clinical and aesthetic effectiveness, with a two-year follow-up. Methods: A 30-year-old non-smoking female patient with an uneventful medical history was referred to the Implantology Clinic at Paulista University, São Paulo, with a compromised maxillary lateral incisor, and complaining of masticatory parafunction and aesthetic issues. Despite satisfactory oral hygiene, intraoral examination showed advanced local tissue destruction with severe alveolar bone loss and dental mobility. A large buccal plate dehiscence was detected clinically and radiographically. A non-traumatic surgical approach under local anaesthesia consisted of simple manual tooth removal, requiring no forceps or elevators. After 30 days of healing, a cone beam CT showed lingual bone width of 3mm. An implant (3.25 x 13mm Biomet-3i) was installed in the basal bone adjunctively with a mixture of particulate autologous bone graft harvested from mandibular body cortical bone and BioOss[tm] xenogeneic bone graft (to reconstruct the horizontal defect). A preadapted titanium mesh (Neobiotech[TM]) and resorbable collagen barrier (BioGide[TM]) were placed over the grafted region to help maintain bone volume and prevent any exposures. During a six-month healing period, the patient used a provisional removable partial denture. Then the titanium mesh was removed and a provisional crown was fabricated to optimise the emergence profile. Results: No bone exposure was observed in the grafted area and no complications occurred in the donor site. Postoperative clinical and CT examinations at 6, 12 and 24 months showed sufficient and satisfactory bone formation. Besides the limited torque (15N/cm) during implant placement, the final prosthetic design was successful. At two-year follow-up, volumetric stability and satisfactory functional and aesthetic results were achieved. Conclusion: Mixed bone grafts combined with titanium mesh appear to be an effective and advantageous procedure for horizontal bone defects in aesthetic zones, providing volumetric stability and satisfactory functional and aesthetic results.









