-
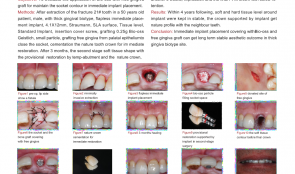

APPLICATION OF BIO-OSS WITH FREE GINGIVA GRAFT FOR MAINTAINING SOCKET CONTOUR IN IMMEDIATE IMPLANT PLACEMENT
Objectives: To evaluate the application of BioOss with free gingival graft for maintaining the socket contour in immediate placement of implants. Methods: After extraction of a fractured 21# tooth in a 50-year-old male patient, with thick gingival biotype, a flapless immediate placement implant (4.1 mm x 12mm Straumänn SLA was inserted to the tissue level of a standard implant, and covered with an insertion screw. Grafting was with 0.25g Bio-Oss small particles, using free gingiva graft from palatal epithelium to close the socket. The natural tooth was cemented with a crown for immediate restoration . After 3 months, the second-stage soft tissue was shaped with provisional restoration by temporary abutment and the natural crown. After another 6 weeks, impressions were taken and the final PFM (porcelain-fused-to-metal) crown was fixed with screw retention. Results: Within 4 years, the soft and hard tissue levels around the implant were stable, and the crown was supported by the implant with a natural profile with the neighbouring teeth. Conclusion: Immediate implant placement covered with BioOss and free gingiva graft can result in a long-term stable aesthetic outcome in patients with thick gingiva sites. -


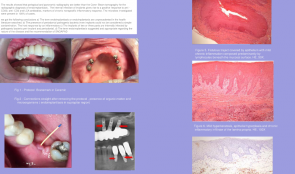
EFFECT OF A 0.2 % HYALURONAN-CONTAINING GEL ON ALVEOLAR BONE REMODELLING IN RATS WITH EXPERIMENTAL PERIODONTITIS
Objectives: Hyaluronic acid (HA) is a naturally occurring linear polysaccharide of the extracellular matrix of connective tissue and other tissues. It has several physiological and structural functions, accelerating bone regeneration by means of chemotaxis, proliferation and successive differentiation of mesenchymal cells. The purpose of this study was to evaluate the effect of topical application of a 0.2% hyaluronan-containing gel on bone remodelling in the mandible of rats. Methods: Thirty-two white Wistar rats (weighing 350–450 g and aged 4 months) were divided into three groups: group 1 comprised intact rats (control); group 2 comprised rats with a “peroxide” model of periodontitis, reproduced by a 60-day diet of over-oxidised sunflower oil (model); and G3 comprised rats with peroxide-induced periodontitis that were given topical HA-gel on the gingiva daily for 14 days (treatment). Alveolar bone remodelling was evaluated by biochemical and histologic analysis, and activity of alkaline phosphatase (ALP; an indicator of osteoblastic activity) and tartrate-resistant acid phosphatase (TRAP; a biomarker of osteoclasts) were measured in the alveolar bone. Results: The enzyme activity in alveolar bone was significantly higher in the treatment group than the model group, with levels of 42.56 ± 3.96 mckat/kg and 79.94 ± 3.17 mckat/kg (p Conclusion: The results suggest that topical application of a 0.2% HA-containing gel applied to the gingiva in rats has an osteoinductive effect. -


MODELLING CRITICAL-SIZED BONE DEFECTS IN RABBIT MANDIBLE: A MORPHOLOGICAL STUDY OF BONE HEALING
Objectives: There is little consistency in the choice of appropriate animal models in bone research, where evaluating bone repair dynamics is a basic part of bone morphofunctional studies. Among the available models, rabbits have several advantages. The bone defect repair rate is mainly dependent on the size of the bone wound, and experimentally created osseous injuries for studying repair mechanisms should be wide enough to preclude spontaneous healing. This study aimed to assess bone healing histologically in rabbit mandible defects. Methods: Three adult male rabbits were used. Defects with diameters of 3mm and 6mm, and a depth of 1.5mm, were created by excision of the mandible cortex using a trephine. Defects were allowed to fill with blood and the overlying soft tissues were repaired. Postoperatively, the rabbits were given antibiotic and analgesic therapy. In order to assess osteogenic activity, vital fluorochromic bone markers were used. After 6 weeks surgery, the animals were euthanised and bone segments were dissected and processed for histological evaluation. Analysis was performed with a light microscope. Results: During the observation period, the animals were healthy and presented no signs of infection. Both sagittal and transverse sections showed the dynamic of injury healing. After 6 weeks, the 3-mm defect had completely healed without inflammation, with proliferation of fibrous connective tissue and a minimal amount of immature woven bone. The new bone contained numerous blood vessels and osteoblasts. The 6-mm defect did not fully heal. Bone repair tissue was characterised by woven fibres, consistent with immature primary bone, and primitive Haversian spaces. Conclusion: We investigated the kinetics of healing in different sizes of rabbit mandibular defects. The 6-mm defect was the critical-sized defect. This experimental model will allow evaluation of the effect of different biomaterials on the healing process, in terms of adequacy of tissue quantity and quality, as well as the osteoconductive and osteoinductive characteristics of the test materials. -


ROOT APPROXIMATION AND PENETRATION OF MAXILLARY SINUS AND ITS INFLUENCE ON POST-EXTRACTION OROANTRAL COMMUNICATION— A NOVEL TECHNIQUE FOR OROANTRAL COMMUNICATION REPAIR, AUGMENTATION, AND FINAL RESTORATION
Objectives: The objective of this study was to evaluate the approximation of maxillary tooth roots to the sinus, the incidence of root penetration into the sinus, and its influence on extraction of maxillary posterior teeth. A technique for repairing oroantral communication aimed to augment the extraction site and provide valuable bone volume for implant insertion and final restoration. Methods: Forty-six patients were evaluated by x-ray and perpendicular measurement of sinus approximation from the tip of the root of the posterior teeth to the sinus. The number of root penetration into the sinus were counted. Ten cases had oroantral communications post-extraction and were enrolled in the study. The repair intervention was delayed in two, and eight were operated on at the time of extraction. Sinus floor was elevated noninvasively through the socket and collagen matrix was inserted into the lateral wall of the sinus and rotated to close the oroantral communication of the palatal wall. Corticocancellous bone chips were used to augment the site. Collagen matrix was used again to cover the site, with soft tissue closure. The sites were evaluated by x-ray four months later, to evaluate bone volume and density. Implants were inserted and final restoration was done after four months. The average follow-up of patients as 2.5 years. Results: Both the left and right sides were evaluated for sinus approximation and root penetration. The combined average distances were recorded for the upper first premolars (9.4mm), upper second premolars (4.55mm), upper first molars (4.065mm), upper second molars (1.87mm) and upper third molars (3.6mm). The mean percentage penetration was calculated for the upper first premolars (1.25%), upper second premolars (8.53%), upper first molars (46.4%), upper second molars (27.65%) and upper third molars (21.82%). In this case series, all oroantral communications were successfully closed and all sites were augmented without postoperative complications. Clinical and radiographic evaluations revealed successful implant restoration. Conclusion: Within the limitations of this study, oroantral communications can be repaired and augmented for implant restoration by proper preoperative evaluation of sinus approximation using this novel technique. -


PERI-IMPLANT SOFT TISSUE STABILITY AFTER SINGLE IMPLANT RESTORATION USING EITHER GUIDED BONE REGENERATION OR A CONNECTIVE TISSUE GRAFT . A RANDOMIZED CLINICAL TRIAL
Objectives: The primary purpose was to compare two different surgical procedures: the connective tissue graft and the GBR technique, in conjunction with implant placement. A secondary aim was to assess the influence of the two different procedures on periodontal soft tissue stability of teeth adjacent to the implant site. The null hypothesis was that connective tissue grafting procedures can produce similar clinical results to GBR. Methods: A total of 32 patients were included in the study. Prosthetic stage was scheduled after 6 months from implant insertion. Results: Between-group (test versus control) differences in buccal mucosa thickness were not statistically significant (p = 0. 669). Both groups showed statistically significant differences in changes over time (p = 0.023), with a statistically significant increase in mucosal thickness between T0 and T1 (p = 0.021). There were statistically significant intra-group differences in keratinised tissue height at the implant sites (p Conclusion: The one-year results of this clinical trial on 32 consecutively treated patients confirmed previously published data at 1 and 3 years. The measured clinical parameters indicated healthy and stable peri-implant soft tissue over time in both the test and control groups. Similar results were found for adjacent teeth, thus it may be argued that the coronal reposition of the envelope flap maintains the stability of periodontal tissues following both bone and connective tissue grafting procedures. Within the limitations of this study, it can be concluded that the connective tissue graft procedure was beneficial in maintaining facial gingival level when performed in conjunction with implant placement, showing no statistically significant differences in term of mucosal shrinkage with GBR. -


HISTOLOGICAL ANALYSIS OF CORES OBTAINED DURING IMPLANT PLACEMENT IN SITES WITH PREVIOUS LATERAL MAXILLARY SINUS FLOOR LIFT
Objectives: Recent studies using PCR and RT -PCR analysis has verified that the internal structures of implants and abutmant are heavily contaminated with pathogenic bacteria. The purpose of this study and topographic characterization of the internal spaces (Endoimplanto) of the implants using 2D and 3D computed microtomography. Methods: Six implants Biomet External hexagon cylindrical implants with tapered apex (3.75.0 x 11.5 mm Pi-Brånemark, EXOPRO, Bauru, Brazil) were used to test. Inner structure of implants and abutmant was divided into 4 zones: Endoimplanto/UCLA, Endoimplanto/Abutment, Endoimplanto/Microgap, EndoImplanto/Implants. All micro-CT scans were acquired on a Triumph multi-modality system (Gamma Medica, Northridge, CA) using the following acquisition parameters: tube voltage 80 kVp, tube current 250 A, detector pixel size 50 m, focal spot size 50 m and a field-of-view of 59 or 93 mm. The spatial resolution was 39 m and 28 m, and the radiation dose was 8.3 cGy and 19.7 cGy for a field-of-view of 93 mm and 59 mm, respectively. Results: The results showed that the endoimplanto abutment/UCLA corresponds to 40/50%, Endoimplanto/Abutment 10-20% , Endoimplanto/Microgap 2-3 %, Endoimplanto/Implant 10 -15 % of full structucture implant/Abutment /UCLA. Conclusion: It concludes that the empty spaces of the implants (Endoimplanto ) occupy a large part of the overall volume Implant /Abutment /UCLA. This space can serve as a repository of relevant bacteria and fungi in the development of periodontal and peri-implant disease. The microtomography and a good non -destructive and non-invasive method to search the internal structures of the implants. -


PERIOSTEAL PREFABRICATION OF VASCULARISED CAD/CAM BONE SCAFFOLDS
Objectives: Reconstruction and prosthetic rehabilitation of patients presenting with severely atrophied alveolar ridges or critical-size bone defects of the facial skeleton are clinically challenging. Bone tissue engineering with patient-specific scaffolds are a promising alternative for overcoming the drawbacks of autologous bone grafts. Early neovascularisation and reliable vertical bone height are both crucial for successful implantation, and present the major challenge of these constructs. The aim of this study was to evaluate the neovascularisation potential and bone-forming capacity of a CAD/CAM-designed artificial space (bioreactor) between the medial femur condyle and its periosteum on bioresorbable scaffold structures. Methods: Four skeletally mature Swiss alpine sheep were used. The bioreactor, composed of a PEEK construct (side walls), a vascular pedicle flap (roof) and deperiosted compacta (floor), was locked into position by two 2.4 standard screws. The sheep were put in two groups of two: in the treatment group, the created rectangular space was filled with a bioresorbable β-tricalcium phosphate (β-TCP) scaffold; in the other group, the bioreactor was left empty (negative control). Micro-CT scans were performed immediately and 12 weeks postoperatively. Fluorochrome labelling was performed with calcein green after 4 weeks, and with Xylenol orange after 8 weeks to document new bone formation. Animals were euthanised 12 weeks postoperatively and surgery sites were examined histologically using eosin–Giemsa with pre-mortal intravascular injection of Indian Ink to visualise blood vessels. Results: Fluorochrome labelling displayed moderate early bone formation after 4 weeks with already in-growth into the bioreactor. After 8 weeks, there was pronounced new bone formation in the bioreactor. After 12 weeks, eosin–Giemsa staining showed degradation and bony replacement of the scaffold material, bone in-growth into the scaffold voids, and extended neo-vascularisation into the scaffold originating from the periosteal flap. Micro-CT data showed that after 12 weeks of implantation, 45% of the region of interest (ROI) contained new vertical bone-like tissue composed of new bone and ossified scaffold material. The overall volume increase of bone-like tissue in the ROI was +9% and the calcification level increased by 30%. Conclusion: These results indicate that the bioreactor concept strongly promotes new bone formation, ossification and extended vascularisation of the scaffold material. The newly formed bone is highly calcified and thus of ideal quality for implantation purposes. -


VOLUMETRIC SOFT-TISSUE CHANGES WITH THREE DIFFERENT RIDGE AUGMENTATION PROCEDURES—AN EXPERIMENTAL STUDY IN BEAGLE DOGS
Objectives: Guided bone regeneration by means of membranes and bone substitutes is one of the most documented approaches for restoring deficient alveolar ridges. Despite routine use of the techniques, it is not known to what extent these approaches can restore the tissue volume lost after tooth extraction. The aim of this study was to analyse the volume loss occurring after extraction and how much lost volume can be recovered by three different bone augmentation procedures. Methods: To create the alveolar ridge defects, the teeth were sectioned in a buccal–lingual direction at the furcation level, and the mesial roots of M1 and P4 and distal roots of P3, P2 and P1 (monoradicular) were individually extracted. Three vertical grooves of about 6mm in height and 6mm in depth (as far as the lingual cortical bone) were prepared in order to eliminate the buccal bone plate. After 12 weeks, the dogs were randomly assigned to one of three regenerative procedures: graft-only (B) in which the defect was filled with a particulate bone substitute (Bio-Oss Collagen); membrane only (M) in which the defect was covered with a bioabsorbable collagen membrane (Bio-Gide); and combination group (T) in which the defect was filled with a particulate bone substitute (Bio-Oss Collagen) and membrane was added. Conventional polyvinyl impressions were taken before extraction and defect creation at one time point (T1), before regenerative surgery (T2) and after 3 months of healing (T3). The cast models were optically scanned to obtain stereolithography (STL) files. Linear and volumetric measurements included volumetric analysis, distance between surfaces, and tissue thickness at three levels below the alveolar ridge on the buccal side of the regenerated site(at 1, 3 and 5mm). Results: A total of 18 casts were obtained at T1, with 18 at T2 and 9 at T3. No impressions were taken at the time of sacrifice to avoid disturbing early healing. The box-shaped defects were effective in creating horizontal and vertical ridge deformities (comparison T1–T2). None of the three regenerative approaches resulted in complete reconstitution of the alveolar ridge to baseline dimensions (comparison T1–T3), although volume gain in groups B and T was significantly better than in groupM (comparison T2–T3). Conclusion: The three regenerative approaches failed to rebuild the post-extraction loss in tissue volume. -

ENDOIMPLANTIASIS: DESCRIPTION OF THE CLINICAL ASPECT, RADIOGRAPHIC, HISTOLOGIC, IMMUNOHISTOCHEMICAL AND MICROBIOLOGICAL – A CASE SERIES
Objectives: Recent in vivo studies on the performance in sealing ability in all prosthetic platforms are disappointing from a biological point of view of biosafety, known pathogenic bacteria for periodontal disease and periimplantitis colonize inner of the implants and abutment. The aim of this study is to demonstrate that the internal colonization of the implants in vivo pathogenic bacteria should be considered a new infectious disease and not a simple contamination. Methods: In four clinical cases were performed clinical, periapical, panoramic radiography and Cone-Beam tomography. Hematoxylin and Eosin and Immunohistochemistry stain was used to investigate the inflammatory infiltrates (Anti-CD20 and Anti-CD3). Quantitative real-time polymerase chain reaction (PCR) was carried out for counts of 5 microorganisms; Aggregatibacter actinomycetemcomitans, Porphyromona gingivalis, Tanerella forsythia, Tanerella denticola, Prevotela intermedia. The Standardised Nomenclature of Animal Parasitic Diseases (SNOAPAD) was used to define the nomenclature of the disease. We searched the MEDLINE (PubMed), LILACS, Google and SciELO databases using the descriptors "endoimplantiasis" and "endoimplantosis" and no time limits. Results: The results showed that periapical and panoramic radiography are better than the Cone- Beam tomography for the radiographic diagnosis of endoimplantíasis . The internal infection of implants gives rise to a positive response to anti -CD20, anti -CD3 and LCA antibodies, markers of chronic nonspecific inflammatory response. The microbes investigated were present in 100% of cases. Conclusion: We draw the following conclusions a) The term endoimplantiasis or endoimplantosis are unprecedented in the health literature searched. b) The presence of periodontal pathogenic bacteria inner implants could not be considered a simple contamination. The host response by an inflammatory c) The implants of two or three parts are internally infected by pathogenic bacteria peri-implant and periodontal. d) The term endoimplantiasis suggested and appropriate regarding the nature of the disease and the recommendation of SNOAPAD. -
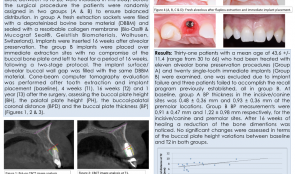

ALVEOLAR DIMENSIONAL VARIATIONS IN ALVEOLAR PRESERVATION AND POST-EXTRACTION IMMEDIATE MAXILLARY IMPLANTS—A 3-D MULTILEVEL MULTIVARIATE PROSPECTIVE STUDY
Objectives: The aim of the study was to evaluate the bone dimensional alterations that occur following tooth extraction and immediate or secondary implant installation in the maxillary arch, and the factors that may influence it, through assessment of early healing events and dimensional changes of the buccal and lingual walls of fresh extraction sockets following immediate implant installation compared to alveolar preservation and secondary implant placement. Methods: Thirty-five patients (mean age 49.58 ± 11.09 years) treated with 37 single-tooth implants in the maxillary area (from 15 to 25) were included in this study. Before surgery, patients were randomly assigned to two groups to ensure balanced distribution. In group A, fresh extraction sockets were filled with Bio-OssTMdeproteinised bovine bone material (DBBM) and sealed with a resorbable collagen membrane (Mucograf SealTM). Implants were inserted 16 weeks after alveolar preservation. In group B, implants were placed over immediate extraction sites with no compromise of the buccal bone plate and left to heal for a period of 16 weeks, following a two-stage protocol. The implant surface–alveolar buccal wall gap was filled with the same DBBM material. Cone-beam CT was performed after extraction and implant placement (baseline), and at 4 weeks (T1), 16 weeks (T2) and 1 year (T3) after surgery, to assess buccal plate height (BH), palatal plate height (PH), buccal–palatal coronal distance (BPD) and buccal plate thickness (BPT). Mean values of each groups were compared using a t-test and ANOVA for comparison of multiple variables. A Pearson correlation analysis assessed the influence of the alveolar anatomy and extension of bone resorption in at different time sets. Statistical significance was set at 0.05. Results: Thirty-one patients (mean age 43.6 ± 11.4 years; range 30–66) treated with thirteen alveolar bone preservation procedures (Group A) and twenty single-tooth immediate implants (Group B) were examined. Of the initial thirty-five patients, one was excluded due to implant failure and three failed did not finish the recall program (all were in group B). At baseline, group A had BPT at the incisive/canine sites of 0.48 ± 0, 36mm, and 0.93 ± 0.36mm at premolar locations. Group B had BPT of 0.91 ± 0.47mm and 1.22 ± 0.98mm for the incisive/canine and premolar sites, respectively. A normal distribution was found for both groups regarding BPT. At T2, there was a reduction in bone dimensions. No significant changes were found in BH between baseline and T2 in either group. Significant differences were found in BPD from baseline to T1 and from baseline to T2, with a statistically significant reduction in buccal–palatal volume in both groups. A positive correlation was found between BPT and the reduction in buccal–palatal volume, described by the BPD measurements, in both groups. Conclusion: Both treatments failed to prevent bone resorption. Immediate implant installation in fresh sockets with DBBM particles was no better than alveolar bone preservation in terms of bone preservation of fresh extraction sockets, but both treatments reduced bone loss after extraction compared to non-grafted sites (described in the literature), and may help clinicians to make decisions about immediate implant placement into sockets. Future studies might compare this type of placement with other treatments in the anterior maxillary region, and consider different timings of placement and related surgical procedures.









