-


UNRAVELLING THE PROGRESSION TOWARDS PERI-IMPLANTITIS MICROCOSM AND DISINFECTION DYNAMICS ON TITANIUM IMPLANT SURFACES
Objectives: Biofilms contamination of implant surfaces are part of the aetiology of peri-implantitis, and different surface decontamination techniques have been proposed as anti-infective therapy. However, no single intervention has been found to be superior. The focus of the present study was to explore the microbial ecology of the peri-implantitis microcosm, and to develop novel surface decontamination methods. Methods: Microcosm biofilms were grown for 30 days in a constant depth film fermenter (CDFF) on SLA andmTi discs, under standardised parameters associated with peri-implantitis. The discs were randomly allocated to three test groups (T1, T2, T3), and two control groups, one consisting of discs with undisturbed peri-implantitis microcosm biofilms (MC) and one with sterile discs (SC). The test group T1 underwent mechanical cleaning with a TiBrushTM (TiB); T2 underwent a combination of TiB and photodynamic therapy (PDT); and T3 underwent a combination of TiB and 0.2% chlorhexidine gluconate/1% sodium hypochlorate (CA). The biofilms were visualised under confocal laser scanning microscopy and surface chemistry was evaluated by scanning electron microscopy with energy dispersive x-ray analysis (SEM/EDX) and X-ray photoelectron spectroscopy (XPS). The bacterial composition of the biofilms was studied before and after disinfection by next-generation sequencing (NGS) of 16S rRNA gene amplicons (MiSeq). Cytocompatibility testing was carried out using AdB Serotech and endotoxin testing bacterial by Kinetic-QCL. Image J and CasaXPS were used for image analysis. Results: The CDFF peri-implantitis model presented here favoured the growth of higher proportions of Klebsiella, Prevotella, Parvimonas, Porphyromonadaceae (family), Actinomyces, Fusobacterium, Enterobacteriaceae (family), Lachno anaerobaculum and Corynebacterium in in vitro peri-implantitis conditions. ISO-surface-volume rendering and analysis of the confocal biofilm stacks revealed the complex microstructure of the undisturbed MC. The physicochemical composition of titanium surfaces before and after decontamination was also investigated, as well as the biocompatibility effect when cultured with MG-63 cells. Elemental analysis disclosed surface alterations of the discs undergoing different treatments. Endotoxin was found in MC and all test groups. The highest levels were found in M surfaces (MC: 12,000 UI/mL). The core microbiome differed between M and SLA surfaces. Bacteria were observed in all groups after disinfection. Streptococcus were present in all SLA- and M-treated samples. Overall, M surfaces were contaminated by Prevotella, Parvimonas, Klebsiella and Neisseria in the highest proportions. Conclusion: The CDFF is useful for modelling microbial shifts associated with peri-implantitis pathogen communities. It seems that the titanium substrata plays only a minor role in the development of mature biofilms. Our data suggest that no treatment modality hindered biocompatibility of the titanium surface. The bacteria were mainly composed of gram-negative species and Streptococcus, which prevailed after chemical and mechanical therapy and LPS was found in all experimental groups. Collectively, these results suggest that a successful treatment for peri-implantitis should be holistic, eliminating live bacteria and bacterial virulence factors, and take account of alterations in the titanium surface. The state of the titanium oxide layer following disinfection and host interactions biofilms warrant further investigation. -


CONSERVATION OF BONE ADAPTIVE OPPORTUNITIES DURING ORAL OSTEOPLASTIC SURGICAL INTERVENTION
Objectives: From analysis of the literature, the absence of epithelial proliferation and adaptive capacity dice determines the ability of tissues to regenerate. When planning a clinical experiment, we suggested the presence of gap (≥ 8.0mm) between the implant and the bone in the area of the implant platform (factor of epithelial proliferation). The aim of this study was to evaluate the efficiency of the rooting implant method in terms of preserving alveolar bone volume. Methods: Sixty patients were studied in 2013–2016 (male–female ratio 1:2; mean age 43 ± 5 years). Various parameters were explored using specialist devices such as a physiodispenser. The implant position was determined using a Navigator YUK-MTM (patent number UА 85876), and bone architecture was visualised using modified radiovisiographs with cadmium–zinc–tellurium single-crystal filters. Implants with an internal connection of depth 3.5mm and length 10.0mm were used. Patients were divided into two groups. The treatment group (n = 30) underwent root implant surgery, with the application of bone thickening gel-like material on the back of the circular platform implant. When rooting compression of this layer reached a thickness of 0.5mm as displayed on the navigational device, the operation was stopped. The back implant surface and surrounding area were covered with a 10.0-mm nanostructured membrane. The control group (n = 30) underwent standard dental implantation. Surgery was carried out by a single operator under standardised conditions, and all patients were examined by a standard procedure. The degree of vertical bone resorption after 6 and 12 months was used to indicate bone atrophy. Results: After 6 months, the treatment group gave unexpected result: in sixteen cases, there was vertical restoration of bone tissue in the near-implant area. In nine, excess bone tissue, freeing the cap implant, was removed. In ten cases, the initial bone level was preserved at the near-implant area. Changes in gums and problems with subsequent prosthetics occurred significantly less often. In four cases, bone was resorbed approximately 1.5mm from the lingual and vestibular sides of the alveolar crest. After 12 months, the patients in the treatment group showed no bone loss. In 22 patients in the control group (73%), X-ray and visual examination revealed varying degrees of proliferation of soft-tissue defect in the area of the periosteum (which can be affected by watering), whereby defects covered the implants irregularly. Radiovisiographic images of both groups revealed 46 cases with wedge-shaped defects filled with gingival tissue (the fine bone structure was not visible using standard methods). The navigation device gave an accuracy of implant positioning 2.0 ± 0.5 minutes (at a deviation of less than 25 arcminutes) and 1.0±0.5 minutes (at a deviation of less than 5 minutes). Linear positioning accuracy was 0.50 ± 0.05mm (at the implant moving up to 10mm). Conclusion: It is possible to predict the impact of pathogenic factors in dental implantation and safely achieve prosthetic restoration of anatomical structures for patients and their organs. Bone regenerative capacity is preserved and bone remodelling is stabilised in the area of the periosteum. The proposed method of visualising thin bone structure makes it possible to assess the impact of surgery on the size and nature of the defect, and predict reparative capabilities and the effectiveness of rehabilitation. The clinical potential of this medical navigation includes dentistry and medical robotic systems. This study opened up further possibilities for optimising the surgical process, predicting the impact of pathogenic factors in dental implants, and eliminating it. -


EFFECTS OF LOW LEVEL LASER THERAPY ON BONE REGENERATION OF INTRABONY DEFECTS – HISTOLOGICAL STUDY
Objectives: The aim of this study is to assess the histological effectiveness of a low level laser therapy (LLLT) with respect to the acceleration of bone regeneration after surgical treatment of intrabony defects. Methods: Twenty patients with intrabony defects, aged between 20-45, non-smokers, good health condition present at the time of the surgery, were randomly divided in two groups. Informed consent was obtained. Each patient had at last one periodontal defect treated by bone allograft. The test group received a postsurgical treatment with low lever laser therapy (LLLT). The equipment used was OsseoPulse AM300 (extra oral light emitting diode), at an intensity of 20mW/cm2 for 20 minutes per day for 21 consecutive days. The control group received no treatment with LLLT. The bone formation were evaluated in both groups at baseline and 6 months postoperative by the means of a biopsy of tissue followed by a histological analysis. Results: The histological study of the control sample harvested 6 months postoperative showed of irregular fragments of bone in loose fibrous connective tissue. The diagnosis of this tissue sample are evaluated to be a vital lamellar bone with chronic inflammation of the narrow spaces. The histological study of the test sample at 6 months after regeneration showed bone formation without inflammatory cells and occasional nonviable bone consistent with regenerating bone. No evidence of the grafted material is present. Conclusion: With all the limitations regarding the number of patients and the follow up period, the histological analysis showed that the intrabony defects regenerated by bone allograft and treated with LLLT produces more significantly bone that the non-treated defects. Histological study suggests that in 6 months there is new bone formation in the defects treated with LLLT. Clinical data indicate the possibility of more rapid wound closure and subsequent healing in zones treated with LLLT as compared with control - inflammatory cells and occasional nonviable bone consistent with regenerating bone. No evidence of the grafted material is present. -


Osteology Monaco 2016 - Poster Presentation
Objectives: Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Methods: Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus estLorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Results: Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est Conclusions: Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et ea rebum. Stet clita kasd gubergren, no sea takimata sanctus est -


HISTOLOGICAL ANALYSIS OF CORES OBTAINED DURING IMPLANT PLACEMENT IN SITES WITH PREVIOUS LATERAL MAXILLARY SINUS FLOOR LIFT
Objectives: To examine histologically the characteristics of the residual material obtained during the placement of dental implants in sites where bone regeneration was previously performed by the procedure of maxillary lateral sinus floor lift, comparing the histological characteristics when a xenograft alone (Geitslich Bio-Oss®) was used versus regenerations where a combination of xenograft and allograft (Bio-Oss®+Puros®) was used. Methods: A descriptive cross-sectional study was conducted according to the established rules of research on human subjects and adjusted to the scientific, technical and administrative standards, with the support of the Research and Ethics Committee of the Faculty of Dentistry at the Pontifical Universidad Javeriana (CIEFOUJ). Analysis of 11 cores obtained from sites that were regenerated by a lateral approach for the elevation of the maxillary sinus floor, 4 cores in control group where a xenograft alone (Geitslich Bio-Oss®) was used and 7 cores in group test (Bio-Oss® + Zimmer Puros®), the samples were obtained from 6 to 12 months after the elevation of the maxillary sinus floor. Histological analysis was performed by an expert pathologist who made observations of the core samples using hematoxylin and eosin staining and polarized light to differentiate structure characteristics, further quantitative analysis was conducted with a public domain Java image processing program (imagej) and an statistical analysis was applied with a Wilcoxon (Mann-Whitney) test. Results: After the samples were processed and analyzed, histologically both groups showed graft particles surrounded by new bone, osteoid cells and osteoblasts. There was graft material in intimate contact with new bone and bone apposition lines with active zones. The control group consistently showed a greater presence of mature cortical new formed bone in comparison to the test group, where the observation showed a more disorganized structure with areas of new formed cancellar bone with areas of cortical bone. The quantitative analysis showed an average of 34% of new bone in control group (xenograft) and 27% in the test group (allograft + xenograft), however the statistical test showed a p value= 0.25. Conclusion: The initial argument of the present study was to analyze histologically the behavior and results of sites regenerated by an effective technique and using clinically proven bone substitutes; and comparing the combination (xenograft + allograft) with the novelty that xenograft alone was used as a control group, being that this design was not reported in common scientific databases at the moment that the study was initiated. Both control and test group resulted in bone resorption and new bone formation, there was not a statistically significant difference between the use of xenograft as a single material or in combination with allograft for maxillary sinus floor lift and subsequent placement of dental implants, also there were no differences in primary stability at the time of placement of the implants. However, the sample size calls for further investigations in order to increase the evidence of the comparison proposed in the present study. -
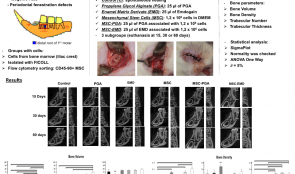

ENAMEL MATRIX DERIVATE (EMD) ON MESENCHYMAL STEM CELLS IN PERIODONTAL REGENERATION: A MICRO-TOMOGRAPHIC ANALYSIS
Objectives: Evaluate the bone formation in periodontal fenestration defects in rats applying bone marrow mesenchymal stem cells (MSC) with or without Enamel Matrix Derivate (EMD). Methods: Periodontal fenestration defects of 2 mm in height, 4 mm in width and 1 mm in depth were created in the mandible of isogenic rats. The animals were allocated into 6 groups and further divided into 3 subgroups for euthanasia at 15, 30 or 60 days postoperative (n=6 for each subgroup). Control Group (C) was the spontaneous healing. In the Propylene Glycol Alginate Group (PGA) 25µl of the vehicle was applied in the defect. The Enamel Matrix Derivate Group (EMD) received 25 µl of Emdogain™. Mesenchymal stem cells (MSC) were collected from the iliac crest of 2 isogenic rats, isolated with Ficoll and cultured in flasks. The cells were separated by flow cytometry to obtain a cell population of CD45-90+ MSC. In the mesenchymal stem cell groups (MSC, MSC-PGA and MSC-EMD) a pellet with 1,2 x 106 cells was applied in each defect, but in MSC-PGA and MSC-EMD groups the pellet was mixed with 25µl of PGA or EMD, respectively. After euthanasia the mandibles were fixed and scanned by computed microtomography apparatus. Bone volume, bone density, trabecular number and thickness were analyzed by SigmaPlot™. The normality of data was checked and ANOVA One-Way test was used, with a significance level of 5%. Results: Bone volume was increased in all groups in all times (p 0.05). In 60 days all groups were similar and had higher volume than PGA (p 0.05) and higher than C, PGA and MSC (p 0.05). MSC-E also had higher number than C and MSC (p 0.05) but statistically larger than C, EMD and PGA (p > 0.05). In 60 days C and EMD had higher thickness than MSC, MSC-PGA and MSC-EMD (p Conclusion: The adhesion of stem cells to EMD resulted in more bone volume in periodontal regeneration defects only in the period of 30 days. However, the bone density and the trabecular number and thickness were either similar or inferior to EMD alone. -


A RANDOMIZED, CONTROLLED CLINICAL TRIAL OF LATERAL RIDGE AUGMENTATION USING AUTOGENOUS BONE BLOCKS OR XENOGENIC BONE BLOCK GRAFTS LOADED WITH RECOMBINANT HUMAN BONE MORPHOGENIC PROTEIN-2)
Objectives: Recent studies using PCR and RT -PCR analysis has verified that the internal structures of implants and abutmant are heavily contaminated with pathogenic bacteria. The purpose of this study and topographic characterization of the internal spaces (Endoimplanto) of the implants using 2D and 3D computed microtomography. Methods: Six implants Biomet External hexagon cylindrical implants with tapered apex (3.75.0 x 11.5 mm Pi-Brånemark, EXOPRO, Bauru, Brazil) were used to test. Inner structure of implants and abutmant was divided into 4 zones: Endoimplanto/UCLA, Endoimplanto/Abutment, Endoimplanto/Microgap, EndoImplanto/Implants. All micro-CT scans were acquired on a Triumph multi-modality system (Gamma Medica, Northridge, CA) using the following acquisition parameters: tube voltage 80 kVp, tube current 250 A, detector pixel size 50 m, focal spot size 50 m and a field-of-view of 59 or 93 mm. The spatial resolution was 39 m and 28 m, and the radiation dose was 8.3 cGy and 19.7 cGy for a field-of-view of 93 mm and 59 mm, respectively. Results: The results showed that the endoimplanto abutment/UCLA corresponds to 40/50%, Endoimplanto/Abutment 10-20% , Endoimplanto/Microgap 2-3 %, Endoimplanto/Implant 10 -15 % of full structucture implant/Abutment /UCLA. Conclusion: It concludes that the empty spaces of the implants (Endoimplanto ) occupy a large part of the overall volume Implant /Abutment /UCLA. This space can serve as a repository of relevant bacteria and fungi in the development of periodontal and peri-implant disease. The microtomography and a good non -destructive and non-invasive method to search the internal structures of the implants. -


Plant-derived Pectin Nanocoatings to Prevent Inflammatory Cellular Response of Osteoblasts following Porphyromonas Gingivalis Infection
Objectives: The aim of the study was to evaluate in vitro the impact of bioengineered plant-derived Rhamnogalacturonan-I’s (RG-I) nanocoatings on osteogenic capacity and pro-inflammatory cytokine response of murine osteoblasts following Porphyromonas gingivalis (P. gingivalis) infection.Bioengineered RG-I’s from pectins are potential candidates for surface nanocoating of medical devices due to their physical, chemical, and biological properties. Methods: Murine osteoblast-like cells (MC3T3-E1) and isolated primary calvarial osteoblast from C57BL/6J (B6J osteoblasts) mice were infected with P. gingivalis and incubated on polystyrene tissue culture plates with or without nanocoatings of unmodified isolated RG-I's from potato pulps (PU) or dearabinanated RG-I's (PA). Cell proliferation, metabolic activity, mineralization and osteogenic and pro-inflammatory gene expression were examined at different time points and repeated six times each (n = 6). Results: Following P. gingivalis infection, MC3T3-E1 and B6J osteoblasts cell proliferation after 12, 24, 48 and 72 hours was significantly higher when cultured on PA but not PU coating as compared to cells cultured on control surface without nanocoating. Cell metabolic activity after 3, 7, 14 and 21 days was significantly enhanced in MC3T3-E1 and B6J osteoblasts cultures on surface coated with PA compared to control; on surface coated with PU in MC3T3 culture. Moreover, P. gingivalis infected MC3T3-E1 and B6J cells formed after 3, 7, 14 and 21 days significantly higher amount of calcium deposits on PA but not PU coating as compared to cells cultured on control surface. Finally, Il-1, Il-6, TNF-alpha and Rankl gene expression were down-regulated after 3, 7, 14 and 21 days in cells cultured on PU and to a higher extent on PA as compared to the corresponding control whereas Runx, Alpl, Col1a1, Bglap were up-regulated vice versa. Conclusion: Our data clearly show that pectin RG-I's nanocoating with high content of galactan (PA) reduces the osteoblastic response to P. gingivalis infection in vitro and may therefore reduce a risk of inflammation especially in immunocompromised patients with rheumatoid or periodontal disorders. -
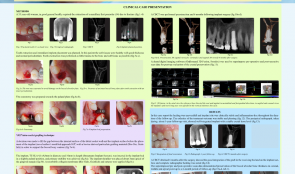

IMMEDIATE FLAPLESS PLACEMENT OF AN IMPLANT IN A MAXILLARY RIGHT FIRST PREMOLAR SITE—CBCT EVALUATION OF FACIAL BONE PRESERVATION USING A NOVEL MODIFIED APPROACH
Objectives: The purpose of this study was to evaluate horizontal zero-dimensional changes of the buccal alveolar plate using cone-beam CT (CBCT) following maxillary premolar single immediate implant placement into fresh extraction socket. A novel intra-socket grafting technique (IGT) was used for placing graft material into the implant–socket gap to minimise the resorptive process. Methods: A 58-year-old woman in good general health required extraction of a maxillary first premolar (1.4) due to fracture, with extraction and immediate implant placement. Her soft tissues were healthy with good thickness and normal periodontium. Extraction involved minimal trauma to the bone and soft tissue. The osteotomy was prepared towards the palatal plate. A decision was made to fill the gap between the internal surface of the labial socket wall and the implant surface before installing the implant by IGT, with bovine-derived particulate grafting material (Bio-OssTM) to support the buccal bony contour. The TE-SLA 4 implant (diameter 4.8 mm, length 10mm) was inserted in the implant bed in a slightly palatal position and primary stability was achieved. The implant shoulder was placed about 3mm apical of the gingival margin. A resorbable collagen membrane (Bio-GideTM) was applied and sutured. Four months after placement, a screw-retained provisional crown was attached to the implant, which was then restored with a cement-retained metal-ceramic crown. CBCT was performed six months after implant surgery and compared with pre-extraction images using imaging software (OnDemand3DTM) to superimpose scan data for evaluation of crestal preservation. Results: Healing was uneventful and the implant site was clinically stable and inflammation-free throughout follow-up. The aesthetic outcome was stable and pleasing. Periapical radiography at the one-year showed a well-integrated implant with stable crestal bone level. CBCT scans taken six months after surgery showed good integration of the graft in the bed and the implant surface, and complete radiographic healing. The scan data revealed preservation of buccal alveolar bone thickness in coronal, middle and apical points after six months, and that using bovine derived-xenograft material to fill the implant–alveolar gap preserved buccal alveolar thickness on the coronal aspect and at the midfacial level, where the buccal width plate is often constricted. Conclusion: Within the limitation of this study, the IGT procedure was associated with horizontal bone stability of the buccal alveolar plate following maxillary premolar single immediate implant placement. The case met the following criteria: i) intact buccal bony plate before and after tooth extraction with an intact periodontium; ii) flapless immediate implant placement procedure; iii) grafting of the implant–socket gap using a bovine-derived bone substitute; iv) placement of the implant towards the palatine bone wall, with adequate primary stability. When these requirements are met, immediate implant placement in fresh extraction socket provides predictable aesthetic outcomes and stable peri-implant tissues. CBCT data clearly demonstrated the preservation of buccal alveolar bone. -


MANDIBULAR CLASS II FURCATION REGENERATION USING A COLLAGEN MEMBRANE ASSOCIATED WITH ANORGANIC BOVINE BONE PLUS PORCINE COLLAGEN—A CASE REPORT WITH TOMOGRAPHIC EVALUATION
Objectives: Reconstructive periodontal therapy aims to re-establish the architecture and function of periodontal supporting structures lost in periodontitis. Previous studies have reported the potential of guided tissue regeneration (GTR) to regenerate periodontal ligament, cementum and alveolar bone. This case report clinically and tomographically evaluates the treatment of a mandibular class II furcation defect using a collagen membrane associated with anorganic bovine bone plus porcine collagen. Methods: A female non-smoking patient aged 47 years required periodontal treatment. At clinical evaluation, tooth #46 presented a mandibular class II buccal furcation defect. Clinical parameters were probing depth (PD), clinical attachment level (CAL), vertical furcation depth (VFD) and horizontal furcation depth (HFD), and tomographic parameters were tomographic horizontal depth (THD) and tomographic vertical depth (TVD). These were recorded at baseline and one year after surgery. Six weeks after the last session of SRP, a GTR procedure was conducted on tooth #46. Following local anesthesia, intrasulcular and vertical releasing incisions were made and mucoperiosteal flaps were reflected. The inner aspect of the flaps was curetted, the osseous defects were debrided, and thorough scaling and root planing (SRP) were performed using Gracey periodontal curettes and ultrasonic scalers. After irrigation with physiologic saline solution, the collagen membrane (Bio-Gide Perio) was trimmed to cover the osseous defect and extended 3mm apically and laterally to the adjacent bone, and the defect completely filled with anorganic bovine bone and porcine collagen (Bio-Oss Collagen). The membrane was positioned and sutured with resorbable sutures. The flap was positioned coronally until it completely covered the membrane, before applying Nylon sutures. Amoxicillin 500 mg, clavulanic acid 125 mg, nimesulide 100 mg and PerioGard rinse were prescribed. Results: Nylon sutures were removed 14 days after surgery. During the one-year healing period, the patient was maintained on a weekly plaque-control programme for the first month, two-weekly for the second and third months, and monthly thereafter. Healing was uneventful, with no membrane exposure or other complications. The changes in clinical parameters from baseline were: PD reduction 2mm (from 3 to 1mm), CAL gain 2mm (from 3mm to 1mm), VFD reduction 3mm (from 4mm to 1mm) and HFD reduction 2mm (from 3mm to 1mm). Tomographic measurements obtained through sagittal and coronal sections cone-beam CT, showed reductions in THD from 2. 3mm to 1mm and in TVD from 3. 2mm to 1. 4mm. The clinical percentages of defect fill were 75.0% for VFD and 66.66% for HFD; the tomographic percentages of defect fill were 56.52% for THD and 56.25% for TVD. Conclusion: The association of Bio-Gide Perio and Bio-Oss Collagen was associated with uneventful healing and significant good results in the treatment of a mandibular class II buccal furcation defect. GTR promoted improvement in both clinical and tomographic parameters, and defect fill of more than 50%.









