-


THE ADVANTAGES OF LOCAL ANESTHESIA DURING GENERAL ANESTHESIA
Objectives: The initial aim of this study was to evaluate the influence of the use of the local anaesthetic articaine before and after dental extractions, on intraoperative pain during general anesthesia, and the subsequent consumption of intraoperative analgesics (Remifentanil) by children receiving oral rehabilitation at the Unit of Ambulatory Surgery and Anaesthesia of the University Hospital of Montpellier, France. Methods: The clinical study protocol evaluated the intraoperative pain of 62 ASA (American Society of Anaesthesiologists) I or II children, during dental extractions under general anesthesia. The children were divided into two groups by randomised simple blind draw. Group 1 received local anaesthetic before extraction. Group 2 received local anaesthetic after extraction. Their pain was objectified through its physiological manifestations: heart rate and arterial blood pressure. Results: The mean age of the boys was 6.55 years and for girls was 5.29 years. Those who received peri-apical local anaesthetic after extraction experienced a significantly higher increase in systolic blood pressure and heart rate (p ≤ 0.05) compared to those who received it before extractions. The mean increase in heart rate was +10.4% for the patients receiving the anaesthetic after extraction. For the group receiving it before, there was a mean decrease in heart rate of –0.7%. The mean increase in systolic blood pressure the anaesthetic-after group was 11.4%, but was only 1.4% in the anaesthetic-before group. These variations were significant (p Conclusion: This study illustrates the advantage of using local anaesthetic before dental surgery during general anesthesia, which limits the rise in systolic blood pressure and heart rate during tooth extraction. The logical consequent decrease of the consumption of intraoperative analgesics is to be evaluated by further studies. -


CLINICAL EVALUATION OF RISK FACTORS RELATED TO MAXILLARY SINUS FLOOR ELEVATION
Objectives: Maxillary sinus floor elevation is a predictable surgical procedure that is commonly used to overcome the limitations of an atrophied alveolar ridge for dental implant placement. For a precise diagnosis, however, it is necessary to understand the systemic or local risk factors that may affect short- or long-term clinical outcomes. In the present study, we evaluated risk factors associated with the procedure and assessed their correlation with clinical results. Methods: A total of 308 patients (207 women; 101 men; 525 implants) were treated with a combination of maxillary sinus floor elevation and dental implant placement. The mean age of the patients was 55.3 years at the time of sinus floor elevation. The observation was performed between 1 year and 14 years after surgery. Both systemic and local risk factors were evaluated. Systemic factors were age, smoking habit, diabetes, respiratory disease and ASA (American Society of Anaesthesiologists) physical status classification. Local factors were residual bone height, periodontitis, degree of atrophy of alveolar ridge (vertical interval of alveolar ridge), implant position, surgical procedure, use of bone substitutes, perforation of the sinus membrane, and exposure of the cover screw. Each risk factor was assessed for correlation with implant failures. All missing implants were categorised as an early failure or a late failure, and risk factors corresponding to early or late failure were assessed. Results: The number of disintegrated or not integrated implants was 34, and the cumulative survival rate was 93.5%. Of the 34 missing implants, 19 were lost before restoration (early failure) and 15 survived after final prostheses were delivered (late failure). Among the systemic risk factors, respiratory disease was correlated with implant failure (p = 0.032). Local risk factors related to implant failure were use of bone substitutes (p = 0.001: hydroxyapatites), exposure of cover screw (p = 0.001), vertical interval of alveolar ridge (p = 0.029) and simultaneous implant placement with sinus lift (residual bone height Conclusion: Among the systemic factors, age, smoking habit, diabetes and ASA physical status of classification did not correlate with implant failure. In addition, local factors such as periodontitis, position of the installed implants and perforation of the sinus membrane did not affect implant survival rates. However, paying particular attention to respiratory disease among the systemic factors and to exposure of the cover screw among local factors may be important for preventing early failure of implants with sinus lift. No systemic risk factor was significantly related to late failure, but it is essential to take account of the surgical procedure, residual bone height, use of bone substitutes and vertical interval of alveolar ridge to forestall late loss of implants that are installed during sinus lift. -


DENTAL IMPLANTS RECOVER AND MAINTAIN BODY TRUNK BALANCE WITH CONTRACTING FOR OCCLUSION
Objectives: Balance of the body trunk is associated with jaw position, occlusal force, muscular balance and vertical dimension. Dental implants are thought to be capable of correcting balance with high reproducibility following the loss of teethIn the present study, prosthetic restorations with dental implants were analysed in terms of correlation to recovery and maintenance of the body trunk balance. Methods: A total of 14 patients were in the study. They had received implant prosthetics at our university hospital, seven for intercalary single- tooth defects of the first molars, and seven for unilateral free-ends. Occlusal information, such as intercuspal contact position and area, contact number and occlusal force, was recorded onto pressure measurement films (Dental Prescale[tm]) and converted into a numerical form by an analyser (Occluzer[tm]) six months after delivery of implant superstructures. Measurements were performed with or without superstructures in each patient, and all cases were evaluated for the influence of dental implants on body sway (Gravicorder[tm]. Bacteriological and pathological parameters of peri-implantitis were analysed in the patients who were engaged to be healthy or contracted peri-implantitis after dental implant treatment. Results: There were no differences in intercuspal contact area, contact number and occlusal force on implant delivery on both contralateral and bilateral sides of dentition, with or without superstructures in the intercalary defect group. On the other hand, implant prostheses in the unilateral free-end group showed an increase in intercuspal contact area, contact number and occlusal force on the delivery side, but not the contralateral side. Notably, intercuspal contact position and area, contact number and occlusal force for the residual teeth on the delivery side were decreased by distributing functional load to the implants. Body sway was improved and tended to be balanced not anteroposteriorly, but laterally, by dental implant treatment only in the unilateral free-end group, although not statistically significantly. Bacterial flora was detected in patients with and without dental implant prosthetics, and peri-implantitis elevated the bacterial flora that are generally observed in, and specific to, periodontitis. Conclusion: Free-end implants increased intercuspal contact area, contact number and total occlusal force, influencing not the contralateral but the implant delivery side. Improved body sway is attributed to stabilised isometric contraction. In this study, the implant prostheses of the free-end group (not intercalary) acquired symmetry in the parameters, attenuating the range of lateral body sway. Therefore, although anteroposterior sway was not influenced, free-end recovery by dental implant prostheses may be associated with stabilising isometric contraction. Peri-implantitis signified an increase in bacterial flora associated with periodontitis, but not the change in spectrum, indicating that periodontitis may be an intimate factor for peri-implantitis. In conclusion, dental implant prostheses improved intercuspal contact area, contact number and occlusal force to recover and maintain body trunk balance. -

ORTHODONTIC BONE-STRETCHING TECHNIQUE FOR ANKYLOSED TEETH AND IMPLANT RELOCATION—PRELIMINARY RESULTS OF A CASE SERIES
Objectives: Severe injuries or biological dysfunction of the periodontal ligament may lead to ankylosis. Osseointegrated implant and ankylosed teeth are very similar, both with the potential for complete immobility. Ankylosis and osseointegration affect dentoalveolar development during growth, and lead to infraposition and aesthetic problems. Relocation of malpositioned ankylosed teeth or implants to correct positions requires surgery. The aim of this study was to evaluate the orthodontic bone-stretching procedure. Methods: A cohort of patients presented with implants in the wrong position (n = 4) or an ankylosed tooth in infraclusion (n = 14). Orthodontic treatment was conducted for dysmorphosis correction, excluding ankylosed teeth or implants. Before surgery, dental CTs were taken to evaluate the positions of adjacent teeth for surgical planning. Under local anesthesia, a full-thickness flap was reclined and two vertical deep corticotomies were performed using piezosurgery (Piezotome 2 SatelecRTM) on either side of the ankylosed tooth or implant. Then the two vertical cuts were connected by making a third cut, subapical to the apex. Immediately after the surgical procedure, orthodontic traction was applied and reactivated every two weeks. Calipers were used to take comparative measures with adjacent teeth during activation of the bone-stretching device. The quantity and speed of the movement were evaluated. At the end of the treatment, control cone-beam CT (CBCT) was performed, and MeshlabRTM software and movements in three dimensions were assessed by CBCT merging. Results: After a period of 3–9 months, each ankylosed tooth or implant had been moved. At the end of the treatment, they were correctly repositioned. In one case in which root resorptions were important, the movement was stopped by a tooth fracture. The analysis showed that the movement began after a minimal period of three weeks and continued until the end of the traction. The duration of treatment depended more on the distance between the incisal edge and the occlusal plane than on traction strength. Repositioning with vertical movement was more difficult than with palatal or vestibular movements and may require second surgery. The control did not demonstrate periodontal pathology after orthodontic bone-stretching. The control CBCT showed tooth or implant repositioning occurred with no problems. Osseointegration was stable for implants. CBCT merging to show bone movement revealed that the implant or ankylosed tooth moved with the neighbouring bone at the same time and in the same direction. The bone-stretching movement led to vertical bone augmentation. While the maxilla developed in a vertical direction, the ankylosed teeth remained more or less in infraocclusion. The individual growth pattern and progression of infraposition varied with age and sex of the patient. Slight over-treatment might compensate for this. Conclusion: The orthodontic bone-stretching technique seems to be viable for relocating ankylosed teeth and implants from a wrong position, but orthodontic preparation is essential and is associated with adequate soft tissue management. Bone-stretching movement led to a vertical bone augmentation. The results with ankylosed teeth and implants may not be stable over time and continuous growth of the patient must be considered when planning treatment. In the future, this technique may enable relocalisation of implants in the wrong position, however more long-term prospective clinical trials are needed to confirm its effectiveness. -


IMMEDIATE IMPLANT PLACEMENT COMBINED WITH TITANIUM GRANULES—5 YEARS OF CLINICAL EXPERIENCE
Objectives: Immediate placement of implants in the aesthetic zone is a commonly performed procedure, with the implant positioned close to the palatal wall. There are different approaches to managing the remaining gap between the implant and the buccal bone plate. This study aimed to evaluate outcome of a gap-filling procedure after five years. Methods: Implants (n = 53) were placed in the region of upper incisors, canines and bicuspids. After placement, a healing abutment with the same diameter as the implant was connected. Titanium granules were mixed with blood, and pushed with gentle pressure into the gap. The healing abutment was removed and replaced by an abutment with a diameter corresponding to the replaced tooth. A temporary crown was fixed to the abutment and adhered to the adjacent teeth. After three months of healing, abutments and temporary crowns were replaced by definite reconstruction. To evaluate the stability of the alveolar process, clinical pictures were taken before extraction and after delivery of the final crown. Measurements were made using the planning model and master cast. Results: The healing period was uneventful for all cases. The restorations gave a healthy gingival margin with no discoloration of soft tissue. All patients were satisfied with the clinical results. There was minimal collapse of the alveolar process but this did not compromise the clinical situation. Conclusion: The results obtained after five years of clinical use justify further use of titanium granules as a gap-filler with this procedure. -
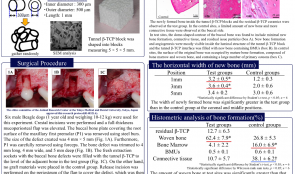

HISTOLOGICAL EVALUATION OF TUNNEL β-TRICALCIUM PHOSPHATE (β-TCP) BLOCKS FOR RIDGE PRESERVATION AFTER TOOTH EXTRACTION WITH BUCCAL BONE DEFICIENCY
Objectives: Alveolar ridge resorption occurs as a consequence of tooth extraction, and bone grafting materials are recommended to reduce these volume changes. In this study, β-TCP blocks were manufactured from randomly organised β-TCP particles with a luminal structure to investigate the effect of these blocks on alveolar ridge preservation after extraction in cases of buccal bone plate deficiency. Methods: Tunnel β-TCP particles are cylindrical with an outer diameter of 500μm, a length of 1mm and a centre hole with an inside diameter of 300 μm. They were manufactured by gathering and fixing randomly organised particles, with a porosity of about 70%, and were shaped into 5 × 5 × 5mm blocks. Six beagle dogs were used. The first premolar of the maxilla was extracted after the buccal bone plate covering the root surface was removed. The extraction sockets with the buccal bone defect were trimmed to 4 ×4 ×5mm (mesiodistal width × buccopalatal width × depth). Bilateral bone defects were filled with tunnel β-TCP blocks at the test sites, and no graft materials were placed in control sites. After two months of healing, histologic and histometric evaluation in the region of interest (ROI) corresponding to the bone defect size was performed. The width and area of new bone formation was measured in the ROI, including bone marrow, basic multicellular units, woven bone formation, and residual TCP. Statistical analysis was performed using the Student’s t-test (p Results: There was no inflammation or wound dehiscence at either experimental or control sites. The new bone formation and residual ß-TCP ceramics were observed inside the tunnel β-TCP blocks at the test sites. Small amounts of new bone and large amounts of connective tissue were observed at control sites. The buccal width of new bone at the test sites was 3.2 ± 0.5, 3.6 ± 0.4 and 3.4 ± 0.2mm at the coronal, middle and apical positions, respectively. For the control sites, the corresponding widths were 1.2 ± 0.3, 2.0 ± 0.6 and 3.0 ± 0.6mm. The width of newly formed bone was significantly greater in the test group, compared to controls, at the coronal and middle positions. The woven bone at the test sites (62.4 ± 7.9%) was significantly higher than that of the controls (26.8 ± 5.3%). The amount of the bone marrow was 4.1 ± 2.2% at test sites and 16.0 ± 6.9% in controls, whereas the amount of connective tissue was 10.7 ± 5.7% at test sites and 38. 1±6. 2% in controls. In both outcome measures, the control sites were significantly higher than the test sites. In terms of the percentage of BMUs, there was no significant difference between the test and control sites (0.5 ± 0.1% and 0.6 ± 0.1%). Conclusion: We compared extraction alone with the use of tunnel β-TCP blocks for alveolar ridge preservation in extraction sockets with buccal bone defects. This is the first study to evaluate the effectiveness of this novel material on ridge preservation after tooth extraction. Clinical healing was uneventful and the material appears to be safe for use in extraction sockets. Histology revealed statistically significant differences between the two groups. The results suggest that ridge preservation using tunnel β-TCP blocks after extraction with deficient buccal bone was effective after two months, but more time is required for replacement by new bone. -


SHORT LIFE OF AN IMPLANT-FIXED PROSTHESIS AND PATIENT SATISFACTION
Objectives: An intercalary defect or free-end defect of a few teeth can be treated with an implant prosthetic. This report introduces an implant treatment with a fixed superstructure delivered to a maxillary edentulous patient who could not accept a removable denture because of a severe gagging reaction, with maintenance of the implant prosthesis for 10 years. Methods: A sixty-one-year-old man complained of a functional disorder with an old, poorly maintained complete denture in 2006. He had been struggling with gagging for a long time. Conventional protocols involve preparing a complete but temporary removable denture was required to determine the occlusal plane and alignment of the artificial teeth, but the patient did not want this. Therefore, we decided to install four implants and prepare a provisional fixed bridge to determine the occlusal indices. Following CT analysis, the implants were manually installed at the lateral incisor and second molar regions bilaterally in one surgical operation. Five months later, further surgery was performed to connect multiunit abutments to the implants. A prosthetic impression was taken at the multiunit abutment level, and a biteplate was used to obtain the occlusal plane and ideal 3-dimensional position of the superstructure. After making adjustments to the provisional superstructure, a final one-piece Pt-Au bridge with a hybrid ceramics–resin coating was delivered. All operations were carried under intravenous sedation. Results: The patient’s maxillary alveolar ridge had been resorbed vertically and horizontally and the buccal side was considerably compromised. For a long time, he had been unable to make continuous use of the complete denture, which covered the palate widely and elicited gagging. Dental CT revealed insufficient bone volume for vertical implant placement, thus a bone graft was required; however, no donor site was identified for posterior augmentation by sinus floor elevation. Therefore, bilateral posterior implants were placed and tilted along the mesial wall of the sinus cavities, to acquire initial stabilisation at 20 N/cm. Two anterior implants were also angled labially to establish the class I occlusion. The initial stability was 25 N/cm. Bilateral mandibular posterior recovery with dental implants and the occlusal plane and vertical dimension were determined by the Willis face method. The patient felt nauseous with the provisional bridge, thus the posterior parts of the bridge were not well maintained, although the patient insisted on continuing with it. Five years later, the patient noticed more frequent bleeding from the peri-implant crevicules. With the pa.ent’s understanding, we decided to remove the whole implants . Conclusion: Multiple tooth defects are often not suited to fixed prostheses on implants because occlusal or functional recovery can be difficult, with restricted implant positions and angulations in absorbed, compromised alveolar ridges and gingival recession. It was difficult for our patient to travel long distances to the hospital at the stated periods, particularly after the onset of respiratory disease, so it informed consent needed to address the predictable insufficiency of the prosthesis, and the increased risk of peri-implantitis. In reality, the patient was satisfied and had no complaints for 10-years, demonstrating that implants can restore function, aesthetics and quality of life, even if they have a relatively short life. -
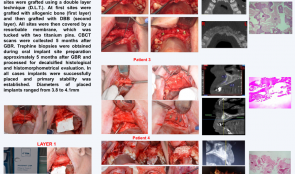

EVALUATION OF A DOUBLE-LAYER TECHNIQUE (DLT) FOR ENHANCING BONE FORMATION IN ATROPHIC MAXILLARY ALVEOLAR RIDGES
Objectives: Different combinations of graft materials have the potential to enhance bone formation in atrophic edentulous or partially edentulous maxilla using guided bone regeneration (GBR) techniques. We aimed to evaluate histologically and radiographically the effect of grafts comprising allogenic bone and deproteinised bovine bone (DBB) in layers, covered with a resorbable membrane. Methods: Five partially edentulous patients with up to 4mm residual bone width in the maxilla underwent GBR. The sites were grafted using a double-layer technique (DLT), with allogenic bone as the first layer and DBB as the second. All sites were then covered by resorbable membrane, tucked into place with two titanium pins. Five months later, cone-beam CT scans were made and trephine biopsies were obtained during preparation of implant sites. These were processed for decalcified histological and histomorphometric evaluation. All implants (with diameters of 3.80–4.1mm) were successfully placed and primary stability was established. Results: The biopsy samples varied in length (4.5– 9mm). Histology showed new bone formation with fragmented medium-sized bone trabeculae within dense fibrous connective tissue and frequent osteoblastic reaction. There were no inflammatory infiltrates. Conclusion: These preliminary results suggest that the double-layer GBR technique gives good, reproducible clinical, radiographic and histological results when used for atrophic maxillary alveolar ridges before placing dental implants. -
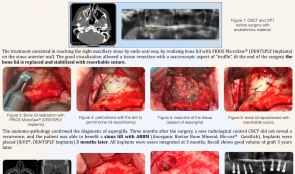

BONE LID APPROACH FOR TREATMENT OF ASPERGILLUS IN MAXILLARY SINUS BEFORE SINUS FLOOR ELEVATION—A CASE REPORT
Objectives: Inserting implants depends on sufficient bone volume. When patients have an osseous defect in the posterior maxillary region, a sinus lift should be necessary. However, sinus pathology, such as Aspergillus infection, is contraindicated for this surgery and must be treated before any sinus lift. Any residue of pathogen that is left in situ is associated with reinfection. The sinus can be accesses via the medial wall, the middle meatus or anterior wall with a buccal section. The Cadwell–Luc technique does not allow conservation of the buccal wall. This study used a surgical procedure with a bone lid for cleaning the sinus before sinus lift and implant surgery. Methods: We report the case of a 58-year-old patient, with no medical or surgical history, who required implant rehabilitation. Radiographic examination revealed complete opacity of the right sinus with material inside. The right maxillary sinus was reached endo-orally, by creating a bone lid with a FRIOS MicroSaw on the sinus anterior wall. Good visualisation allowed resection of tissue with a macroscopic “truffle”. At the end of the surgery the bone lid was replaced and stabilised with resorbable sutures. Results: The anatomopathology confirmed Aspergillus infection. Three months after surgery, new control cone-beam CT found no recurrence, and the patient was able to undergo sinus lift with Bio-Oss anorganic bovine bone mineral (ABBM). XiVE implants were placed three months later and all were osseointegrated after another three months. Good graft volume was observed three years later. Conclusion: Using a bone lid approach for Aspergillus infection of the maxillary sinus allows reconstruction of the buccal wall, and offers good visibility for achieving complete resection of the affected tissue. The bone lid provides excellent intra-sinus access and benefits for future sinus lift and implant surgery. -
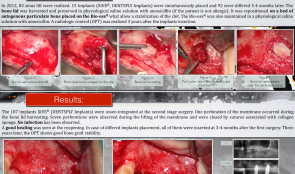

BONE LID FOR CLOSING MAXILLARY SINUS WINDOW DURING SINUS GRAFTING WITH ANORGANIC BOVINE BONE MINERAL (ABBM) AND AMOXICILLIN—3-YEAR FOLLOW-UP OF 83 CASES
Objectives: The objective of this study was to use bone lid with particulate autogenous bone on BioOss ABBM (Bio-Oss) and insert implants just 3–4 months after the intervention, using amoxicillin in physiological saline to prepare the ABBM. Methods: In 2012, 83 cases of sinus lift were performed. Fifteen implants (XiVE) were simultaneously placed and 92 non-simultaneously 3–4 months later. The bone lid was taken during the opening of the buccal wall and preserved in physiological saline solution with amoxicillin (after checking first for allergy). It was repositioned on a bed of autogenous particulate bone placed on the ABBM (to allow stabilisation of the clot), which was also maintained in physiological saline solution with amoxicillin. Panoramic radiographs were carried out 3 years after implant insertion. Results: All 107 implants were osseointegrated at the second-stage surgery. One perforation of the membrane occurred during excision of the bone lid. Seven perforations were observed during the lifting of the membrane and were closed by sutures associated with collagen sponge. No infections were observed and good healing was seen on reopening. In cases of non-simultaneous implant placement, all were inserted 3–4 months after the first surgery. Radiograph images after 3 years showed good bone graft stability. Conclusion: Autogenous bone placed on ABBM allows repositioning of the bone lid and stabilises the blood clot. This seems to accelerate healing of the osseous buccal wall, thus allowing insertion of implants at 3–4 months instead of 6 months. The infection risk is smaller than when using membrane. The use of physiological saline solution associated with amoxicillin to prepare the BioOss seems to be associated with a lower failure rate than that reported in the literature (1.8% versus 14.5%).









