-

Essentials of 3D radiology
Prof. Reinhilde Jacobs and Prof. Marc QuirynenCone beam computer tomography (CBCT) has become an important tool for diagnostics and planning in implant dentistry. This module explains you all the important aspects of the CBCT. -


EVALUATION OF OSTEOGENIC POTENTIAL IN STRO-1-POSITIVE HUMAN TOOTH-GERM DERIVED MESENCHYMAL STEM CELLS (hTGSCs)
Objectives: The objective of this study was compare the osteogenic differentiation potential and mineralisation of STRO-1-positive selected mesenchymal stem cells derived from human tooth germ (hTGSCs) with a heterogeneous hTGSC population, and to determine whether a minor cell subpopulation is more committed to osteogenic differentiation. Methods: Human TGSCs were isolated from dental follicle and apical papilla tissues of impacted tooth germs of third molars from volunteers aged 13–20 years. Cells were expanded and characterised by flow cytometric analysis with CD34, CD45, CD105, CD90, CD44, CD14 and CD117 antigens. Following surface-antigen profiling, STRO-1 antigen, defining a mesenchymal stem cell subpopulation, was used for cell selection with flourescence-activated cell sorting (FACS). Three cell populations (STRO-1 positive, STRO-1 negative, and unsorted) were tested for their ability to differentiate towards osteoblast-like phenotype in osteogenic medium and standard culture medium. Cultures were analysed for cell proliferation (MTS assay and protein assay) and alkaline phosphotase (ALP) activity on days 1, 4, 7, 14 and 21; calcium deposition and gene expression of runx2, osteocalcin and osteonectin with real-time polymerase chain reaction (RT-PCR) on days 7, 14 and 21. Mineralisation and cell phenotype were further screened with Von Kossa staining and confocal microscopy on days 7, 14 and 21. Statistical analysis was made with SPSS Statistics 22[tm]. Kruskal Wallis and Mann–Whitney U tests were applied and a p value of Results: Flow cytometry analysis of passage 3 (p3) hTGSCs showed positivity for CD44, CD90 and CD105, and negativity for CD14, CD45, CD34 and CD117. A total of 11% of p3 hTGSCs were sorted as STRO-1-positive and 24% as STRO-1-negative. In STRO-1-positive cells, osteogenic groups showed significantly higher calcium content than the controls on days 7, 14 and 21. In STRO-1-negative and unsorted cells, the osteogenic groups showed significantly higher calcium content on days 14 and 21 compared to controls. Calcium deposition was not significantly different in osteogenic cell groups in on days 7, 14 and 21. Calcium content seemed to increase in all cell groups from day 7 to day 21. In osteogenic groups, ALP activity of unsorted cells was significantly higher than that of STRO-1-positive and STRO-1-negative groups on days 7, 14 and 21, suggesting a faster rate of osteogenic differentiation in this group, whereas there was no statistical difference between groups on day 21. Activity of ALP was lowest in all groups on day 7 and increased on days 14 and 21. Osteocalcin was expressed in all groups, with no significant difference between them. Osteonectin was highly and significantly expressed in all osteogenic groups on day 7, which is consistent with the findings for ALP and calcium deposition, suggesting that mineralisation was initiated on day 7. Runx2 was downregulated from day 7 to 14. There were no significant differences in the expression of late and early markers of mineralisation in all osteogenic cell groups. Conclusion: Human TGSCs are a novel stem cell source without ethical issues that can be obtained from routine dental treatments. These results suggest they have a high capacityfor osteogenic differentiation. Selecting groups based on STRO-1 negativity or positivity offers no advantages over unsorted cells, but other osteogenic markers might be allow selection of more sensitive osteogenic subpopulations from hTGSCs. -
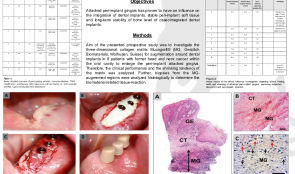

EXPANSION OF THE PERI-IMPLANT ATTACHED GINGIVA WITH A 3-D COLLAGEN MATRIX IN HEAD AND NECK CANCER PATIENTS—RESULTS FROM A PROSPECTIVE CLINICAL AND HISTOLOGICAL STUDY
Objectives: Attached peri-implant gingiva has been proved to influence the integration of dental implants, stable peri-implant soft tissue, and long-term stability of bone leve of osseointegrated dental implants. Methods: The aim of this prospective study was to investigate the 3-D collagen matrix Mucograftä/® for augmentation around dental implants in patients (n = 8) with former head and neck cancer affecting the oral cavity, to enlarge the peri-implant attached gingiva. Clinical performance and shrinking tendency of the matrix were analysed, and biopsies from MG-augmented regions were examined histologically to determine the biomaterial-related tissue-reaction. Results: The participants received a total of 51 dental implants. In all cases, there was uneventful healing without complications or rejection. Six months after vestibuloplasty, there was a mean width of 3.9mm attached peri-implant gingiva with a mean shrinking tendency of 11%. Unrelated to the collagen matrix augmentation, three implants had to be explanted due to peri-implant infection, and dehiscence of the implant windings was observed in two. Histological analysis revealed that the collagen matrix was integrated 8 weeks after vestibuloplasty and augmentation. The compact layer was invaded by mononuclear cells only, towards complete stepwise epithelialisation, and the spongious layer of the matrix was integrated with cell-rich connective tissue involving mononuclear cells alone. Conclusions: Given its limitations, this study revealed that vestibuloplasty with 3-D collagen matrix is a reliable method for enlarging the peri-implant attached gingiva in head and neck cancer patients, with a minimal burden on the patient. Furthermore, the absence of adverse reactions, a favourable tissue reaction, and relatively low shrinking tendency make the collagen matrix a promising alternative to autologous tissue grafts, which are associated with an additional surgical site and post-operative pain. -


MULTINUCLEATED GIANT CELL FORMATION IN DIFFERENT XENOGENEIC BONE SUBSTITUTE MATERIALS—RESULTS FROM AN IN VIVO STUDY
Objectives: Bone substitute materials have become a reliable alternative to autologous bone in augmentation procedures to regenerate lost bone tissue. From previous investigations it is known that origin, processing and physicochemical material characteristics influence the biomaterial-related tissue reaction. This study aimed to analyse and compare tissue reactions to two different xenogeneic bone substitute materials with different preclinical in vivo processing methods. Methods: To evaluate the tissue reaction to the xenogeneic bone substitute materials Bio-OssTM/® and BEGO-OSSTM/®. The substitute materials were implanted subcutaneously in CD-1 mice for up to 60 days. After explantation, biopsies were processed according to a standardised protocol and investigated histologically and histomorphometrically. The focus was on tissue formation, implant bed vascularisation, and the number of multinucleated giant cells within the implant bed. Results: Both bone substitute materials showed good integration within the peri-implant tissue and no signs of adverse inflammatory effects, and both showed increasing vascularisation over the study period. Within the implant bed of the Bio-Ossä/® substitute, a few multinucleated giant cells were observed on the surface of small-sized bone substitute granules in the early integration period. The tissue reaction to the larger granules in the later stages consisted mainly of mononuclear cells. In contrast, the tissue reaction to the xenogeneic substitute BEGO-OSSä/® consisted of biomaterial surface associated multinucleated giant cells. Histomorphometric analysis confirmed the histological results, with significantly more multinucleated giant cells occurring with BEGO-OSSä/®. The increased numbers of multinucleated giant cells also contributed to a greater vascularisation within the BEGO-OSSä/® implant bed. Conclusions: The two xenogeneic bone substitute materials showed distinct tissue reactions, mainly in the formation and migration of multinucleated giant cells. Both biomaterials have the same origin, thus the observed differences seem to relate to different processing techniques and the resulting physicochemical structures. Induction of multinucleated giant cells is associated with formation of unphysiological amounts of fibrous capsule within the implant bed and this might have a negative outcome on integration of the bone substitute and thus on long-term implant stability. Studies are now needed to investigate the clinical relevance of multinucleated giant cells in human bone tissue regeneration. -


ACHIEVEMENT OF A HARMONIOUS SMILE VIA HARD AND SOFT TISSUE MANAGEMENTS ACCOMPANYING IMPLANT-SUPPORTED PROSTHESIS. A CASE REPORT.
Objectives: A perfect appearance is very important for young patients, especially those who lost their anterior teeth through an accident, because it affects their self-confidence and promotes an active social life. Such patients often need professional treatment and psychological support. Methods: After an accident, a 20-year old women was submitted to the Oral Implantology Department at Istanbul University, seeking a good smile and appearance. Clinical examination revealed the loss of her anterior 13,12,11,21 teeth. Deep bite and narrow bone ridge were also observed. Her treatment plans began with a lateral bone augmentation procedure using platelet-rich fibrin (PRF) as a membrane. Two dental implants were placed at anterior 13 and 21 edentulous areas after 4 months, and after another 3 months, the implants were uncovered with placement of adequate keratinised gingiva around the gingival formers. After soft-tissue healing, prosthesis fabrication was begun and completed by screwing in two screw-retained implant-supported porcelain prostheses. Results: The anterior maxilla was successfully restored by two implant-supported, metal-reinforced porcelain prostheses. Conclusions: Multiple factors must be considered to achieve the good final aesthetic results in the anterior maxilla. The choice of surgical procedure, soft tissue management and prosthetic all affect the outcome in aesthetically challenged trauma patients. -


PLATELET-RICH FIBRIN—A PROMISING DRUG DELIVERY SYSTEM FOR TISSUE REGENERATION IN ORAL AND MAXILLOFACIAL SURGERY: PRECLINICAL AND CLINICAL STUDIES
Objectives: The application of cell-based tissue engineering in the form of platelet-rich-fibrin (PRF) is a minimally invasive and cost-effective method to extract cells supporting wound healing and tissue regeneration from peripheral blood. The study aimed to investigate PRF in vitro, in vivo and clinically, in terms of the content, distribution and regenerative capacity of contained cells. Methods: Various in vitro centrifugation protocols have been used to assess cell content and distribution and release of growth factors within solid and fluid PRF. In vivo, both PRF clots and PR solutions were implanted alone or after incubation with collagen membranes into immunodeficient mice. On the clinical side, a range of applications of PRF clots and solutions are reported in tooth extraction, augmentation and decortication in cases of osteonecrosis. Results: The in vitro and in vivo studies clearly showed that changes in centrifuge rotation time and revolutions per minute (r.p.m.) results in different types of cell content. Changing the centrifugation settings also influenced the structure and density of PRF clots. Improved tissue regeneration and healing time were observed in all clinical cases, which were treated with either solid PRF and/or fluid PRF components. Conclusions: PRF can be applied within the operating theatre as a routine-based tissue engineering procedure. Both solid and fluid PRF components can be used clinically for tissue engineering procedures, whereby the surgeon is able to adjust the structure, cell and growth factor content of the PRF constructs to suit a particular clinical need. -


HISTOLOGICAL ANALYSIS OF DIFFERENT COLLAGEN MEMBRANES—PHYSIOLOGICAL OR FOREIGN BODY REACTION?
Objectives: Collagen membranes and matrices are known to be reliable barrier materials in guided tissue and guided bone regeneration, for regenerating lost hard and soft tissues in oral and implant surgery. This study presents results from histological investigations of different collagen-based membranes in order to outline the cellular reactions according to specific characteristics of the materials and their manufacturing processes. Methods: Collagen membranes and 3-D collagen matrices that vary in origin and manufacture were implanted subcutaneously in CD-1 mice and Wistar rats, as well as in humans, to determine the tissue reaction within the peri-implant tissue. Samples extracted up to 60 days after implantation were processed and evaluated histologically and histomorphometrically with a special focus on material stability, vascularisation and induction of a multinucleated giant cells triggered foreign-body reactions. Results: Histology revealed distinct differences in the cellular reactions to the various membranes depending on material-specific characteristics and processing techniques. Cellular reactions consisted mainly of mononuclear cells (e.g. macrophages) as sign of high biocompatibility, material integration and lack of a foreign-body reaction, as well as the presence of multinucleated giant cells that arise from macrophages and migrate into the implant bed. Complete volume stability and integrity was also observed in terms of continuous cell and tissue ingrowth and early vascularisation. Conclusions: Collagen-based membranes serve in periodontology and implantology as versatile barriers that separate different tissues and cells during the healing process. For clinical application of collagen membranes, it is very important to have a detailed knowledge of the cell reactions induced in the implant bed. Cellular reactions, volume stability and membrane permeability, as systematically analysed in this study, have a distinct influence on clinical success. -
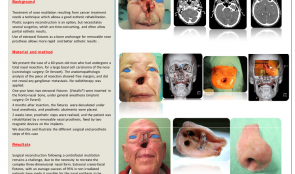

REHABILITATION OF A PATIENT WITH NOSE MUTILATION RESULTING FROM CARCINOLOGIC SURGERY USING EXTRAORAL FIXTURES AND EPITHESIS
Objectives: Treatment of nose mutilation resulting from cancer treatment requires use of a technique that allows good aesthetic rehabilitation. Plastic surgery is an option, but involves several surgeries, which are time consuming and often have only partial aesthetic results. Using an extraoral fixture for bone anchorage of a removable nose prosthesis results in quicker and better aesthetic results. Methods: We present the case of a 60-year-old man who had undergone a total nasal resection for a large basal cell carcinoma of the nose. Anatomopathologic analysis of the resection showed free margins, and did not reveal any ganglionic metastasis. No radiotherapy was applied. One year later, two extraoral fixtures were inserted in the frontonasal bone, under general anaesthesia, and 4 months after insertion, the fixtures were denudated under local anaesthesia, and prosthetic abutments placed. After 2 weeks, prosthetic steps were realised, and the patient received a removable nasal prosthesis that was fixed by two magnetic devices on the implants. This report describes and illustrates the various surgical and prosthetic steps involved. Results: Patient satisfaction was achieved with this technique. Surgical reconstruction following a centrofacial mutilation is challenging because of the need to recreate a complex 3-D nasal form. Extraoral craniofacial fixtures have an average success rate of 95% in non-irradiated patients and have made it possible for the nasal epithesis to be considered as a forerunner in cosmetic rehabilitation strategies. Conclusions: The clinical case presented here shows that transcutaneous extraoral fixtures may be used as bone anchorage for nasal epitheses, in cases of nasal mutilation resulting from cancer treatment. -


COMPARISON OF PERI-IMPLANT BONE LOSS AT IMPLANTS PLACED INTO ALVEOLAR EXTRACTION SOCKETS FILLED WITH ALLOGRAFT AND PLATELET CONCENTRATES AND AT IMPLANTS PLACED IN NATIVE BONE – A RETROSPECTIVE RADIOGRAPHIC STUDY
Objectives: A loss in height and width of the alveolar process takes place after tooth extraction, and there is consensus on the benefits of post-extractional socket filling. The aim of this study was to compare peri-implant bone loss at implants placed in alveolar sockets filled with particulate allogenous bone graft (DFDBA 300–500µm) and platelet concentrates versus implants placed in native bone. Methods: A retrospective clinical study was performed with 84 patients, in whom 247 implants were placed, 169 of which were in native bone (control group) and 78 in socket-grafted bone (DFDBA 300–500µm) and autogenous platelet concentrates (test group). Peri-implant bone loss was measured by two independent operators at 6 and 12 months after placement. A student’s t-test and ANOVA were used to compare bone loss in test and control groups, and correlation coefficients between the two operators were calculated. Results: The overall mesial and distal peri-implant bone loss was 0.9± 0.7mm and 0.9± 0.8mm, respectively, at 6 months, and 1.0± 0.65mm and 1.1± 0.7 mm at 12 months. In the test group, the bone loss was 0.8 ± 0.8 mm at 6 months and 1.2 ± 0.9 mm at 12 months. In the control group, the bone loss was 1.0 ± 0.75mm at 6 months and 1.02± 0.6 mm at 12 months. There was no statistically significant difference between the two groups or between patients with or without history of periodontitis. However, there was a significant difference between the maxillary and mandibular peri-implant bone loss. Maxillary bone loss was greater than mandibular bone loss by an average of 0.2mm at 6 months and 0.4mm at 12 months. There was also a difference between unitary and total edentations (0.7mm at 6 months, 1.2 mm at 12 months) and partial and total edentations (0.5mm at 6 months, 1.2mm at 12 months). Conclusions: From the results of this study we can conclude that peri-implant bone loss in alveolar sockets filled with allogenous bone graft (DFDBA 300–500µm) and autogenous platelet concentrates are similar to peri-implant bone loss in native bone. -
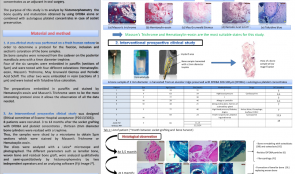

HISTOMORPHOMETRIC EVALUATION OF BONE QUALITY FOR PRESERVATION OF BONE VOLUME AFTER EXTRACTION USING PARTICULATE ALLOGRAFTS (DFDBA) AND PLATELET CONCENTRATES—AN INTERVENTIONAL PROSPECTIVE CLINICAL STUDY
Objectives: There is consensus to preserve bone volume after dental extraction. Some studies show that freeze-dried bone allograft (DFDBA) is the most suitable material for this procedure, and numerous studies support the use of autologous platelet concentrates as an adjuvant in oral surgery. This study aimed to analyse by histomorphometry the quality and maturation of bone obtained using DFDBA alone, or combined with autologous platelet concentrates for socket preservation. Methods: (i) A pre-clinical study on a fresh human cadaver was performed to determine a protocol for fixation, inclusion and staining of bone samples. Six bone samples were removed from the posterior mandibular area with a 4-mm diameter trephine. Four samples were embedded in paraffin (5μm sections) and tested with four different stains: haematoxylin–eosin, Masson’s trichrome, May–Grunewald Giemsa and Periodic Acid Schiff (PAS). Two were embedded in resin (1 μm sections) and tested with toluidine blue. The paraffin-embedded sections stained by haematoxylin–eosin and Masson’s trichrome allowed observation of all the required data. (ii) An interventional prospective clinical study was designed in which eight patients underwent socket grafting with DFDBA and platelet concentrates. After 3–14 months, 2-mm diameter bone cylinders (n = 13) were created with a trephine and sliced in a microtome to obtain 5-μm sections that were stained by Masson’s Trichrome or haematoxylin–eosin. The slices were analysed with a LeicaTM/® microscope and photographed. Evaluated parameters included lamellar bone, woven bone and residual bone graft, and were analysed qualitatively and semiquantitatively by histomorphometry by two independent operators and analysing software (Fiji Image JTM/®). Results: The total new bone area was superior to connective tissue area in all samples (a small proportion of connective tissue and residual DFDBA compared to new bone). Maturation of lamellar bone was observed in 11 out of 12 samples, even after a short post-extraction healing time of 3.5–5 months. Two sections from the same patient also contained bone marrow. Bone remodelling of osteoclasts and osteoblasts occurred in all specimen. No inflammatory infiltrate was detected in any sample. Osteointegration (direct contact with bone) of the DFDBA particles was good in 11 out of 12 samples, and there was progressive resorption and disintegration of the DFDBA particles with time. Fibrocartilage was present in 3 out of 8 patients. Conclusions: Within the limits of these observations on a limited number of patients, it seems that alveolar ridge preservation using particulate DFDBA combined with autologous platelet concentrates allows bone maturation, osseointegration of DFDBA particles, and progressive resorption of DFDBA particles over time. Moreover, fibrocartilage was present in some samples which is an exceptional observation. Further prospective randomised clinical (split mouth) studies are needed with a large number of patients to confirm these observations.









