-

All about Hard Tissue Research - the Research Academy in Kiel
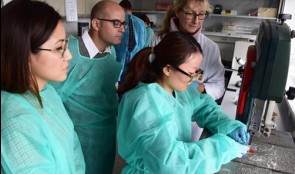
The 13 participants of the intensive course came from 10 countries from all-over the world to gain deeper insights into histology in oral bone regeneration. The Expert Module of the Osteology Research Academy comprises 13 hours of practical (in the laboratory) and 7 hours of theoretical advanced training on the following topics: Pre-clinical and clinical studies in bone regeneration MicroCT, histomorphometry and digital image analysis Bone anatomy, histology, physiology and bone pathophysiology Hard tissue sample preparation Data presentation: from the raw picture to the figure Asked about their experiences during the course the participants gave the following feedback: The professionalism and enthusiasm of all people involved, and the course have been an excellent steppingstone for someone like me who has been out of the research field since my postgraduate studies. Steven Soukoulis, Australia An inspiring course with great content that will be applicable for my future research. Monica Misawa, Brazil In very much enjoyed the workshops, tips and tricks for future projects and the 1:1 discussion with the experts. Dominic Ho, Hong Kong The next Expert Module will take place 7-9. November 2016 in Vienna. Further information For the third time the Osteology Foundation has organised the Osteology Research Academy Expert Module in Kiel. The course on Hard Tissue Research was held in collaboration with the Department of Maxillofacial Surgery at the University of Kiel. -


Expert Council extended
Gustavo Avila-Ortizis Associate Professor with Tenure at the Department of Periodontics at theUniversity of Iowa,USA, and alsoDirector of the Visiting Scholar Program at the same department. He holds a DDS and PhD degree from the University of Granada, Spain, and also a Master degree from the University of Michigan, USA. Gustavos profile in The Box Giorgio Pagniis Periodontistin private practice in Florence, Italy, and instructor at the University of Milan. Hereceived his DDS degree from the University of Firenze, Italy, and holds aMaster degree in Periodontics and Oral Medicine from the University of Michigan, USA. Giorgios profile in The Box The Osteology Expert Council was set up in 2010 in order to expand the Osteology Foundations international network and improve collaboration. Currently, it has 35 members that are a valuable part of the Foundation and drivers for innovative new projects within thethree committees. Both,Gustavo Avila-Ortiz, as well as Giorgio Pagni have already tremendously contributed to past and ongoing projects of the Foundation, in particular to the development of THE BOX. Gustavo Avila-Ortiz (left), and Giorgio Pagni More information about the Osteology Expert Council The Osteology Foundation Board has elected two new members to its Expert Council: Gustavo Avila-Ortiz, USA, and Giorgio Pagni, Italy. Both have already contributed to the Foundations activites over the last years. -

DGI meets Osteology Foundation
At the 30th annual congress of the DGI, the German Society for Implantology (Deutsche Gesellschaft für Implantologie), which will take place on 24 26 November in Hamburg, Germany, the Osteology Foundation will contribute to the program with a session jointly organised with the DGI. The title of the session on Saturday, 26 November, is Science meets everyday practice and comprises presentations as well as interactive discussion. It is chaired by the DGI Committee Nexte Generation and the Osteology Expert Council. Moderators are Frank Schwarz (President DGI, OF Board), Ilja Mihatovic (OF Expert Council, DGI Nexte Generation), and Christian Schmitt (OF Expert Council). The session will be held in German. Registration and further information on the DGI congress website. Programme 11:20 - 11:30 Eröffnung der DGI/Osteology Session Introduction of Osteology Foundation F. Schwarz, Düsseldorf 11:30 - 11:55 Wissenschaft für die tägliche Praxis: Knochenmetabolismus R. Gruber, Wien, A 11:55 - 12:20 Wissenschaft für die tägliche Praxis: Chirurgische Faktoren fr den Langzeiterfolg von Implantaten D. Buser, Bern, CH 12:20 - 12:45 Wissenschaft für die tägliche Praxis: Augmentative Verfahren B. Al-Nawas, Mainz, D 12:45 - 13:10 Interaktive Podiumsdiskussion: Was hat sich klinisch bewhrt und welche Fragen muss die Wissenschaft noch beantworten? -


AAP Collaboration: Workshop Proceedings published
Enhancing Periodontal Health Through Regenerative Procedures Fifty-two workshop participants met in Chicago last summer to conduct a systematic review of existing literature, culminating in the development of consensus reports and practical applications to aid practitioners in the clinical environment. Topics of the workshop included the following: Periodontal Soft Tissue Root Coverage Procedures: Managing gingival recession based on current evidence with a primary outcome goal of complete root coverage Periodontal Soft Tissue Non-Root Coverage Procedures: Assessing the need for gingival augmentation procedures (non-root coverage) around natural teeth Intrabony Defects: Periodontal regenerative strategies for the management of intrabony periodontal defects Furcation Defects: How periodontal furcation defects should be managed via periodontal regenerative therapy and what parameters should be used for treatment selection Emerging Regenerative Approaches for Periodontal Reconstruction: Can emerging technologies for periodontal regeneration become clinical reality? Each practical applications paper describes a specific clinical situation, different approaches that may be considered in its management, and how an expert makes a treatment decision based on the provided evidence. Clinical Advances in Periodontics also offers illustrative images and videos that further detail the clinical situation, how it was managed, and its expected treatment outcomes. How the workshop came to be and what the findings mean for periodontal practice The2014 AAP Regeneration Workshopon the topic Enhancing Periodontal Health Through Regenerative Procedures was of huge interest to the Osteology Foundation, and therefore it was supported with an educational grant. The international consensus meetingwas co-chaired by theOsteology BoardmembersWilliam V. GiannobileandPamela K. McClain. We are excited to announce that the proceedings of this workshop have now been published in a special supplement of the Journal of Periodontology, and are available online with free access. Proceedings of the 2014 AAP Regeneration Workshop The publication is a great result of the first joined efforts of the AAP and the Osteology Foundation. The results havedemonstrated that regenerative procedures are effective and predictable treatment options for helping patients retain their natural dentition. The workshop was an amazing collaborative effort that provides the most current consensus of therapies and technologies in regenerative treatment, sayd AAP president Joan Otomo-Corgel at a press-conference in Chicago, when the publication was announced. Were thrilled to share the results of the these dynamic discussions. This bell weather information will provide tremendous benefit to the periodontal specialty, the dental community, and the patients we treat. -


Osteology Researcher Grants - apply now!
The Osteology Foundation offers besides its established Advanced Researcher Grants a special grant program for young researchers: the Osteology Young Researcher Grants, which support researchers in realizing their own research project and fuelling their research career. The Osteology Young Researcher Grants program (new since 2014) is addressed to all clinicians and researchers (primary investigators) currently undergoing post-graduate education or within three years thereafter. The grants are limited to 30000 Swiss Francs with a maximum project duration of one year. The new Young Researcher Program is dedicated to projects with sound hypothesis, and aims that show thinking out of the box. The Osteology Advanced Researcher Grants program is addressed to clinicians and researchers at universities and in private practice (having an university affiliation) conducting research in the field of dental tissue regeneration. It is dedicated to projects with hypothesis and aims focusing on clinical relevance bolstered with preliminary work within a research group setting. In general, grants are limited to 100000 Swiss francs with a maximum project duration of two years. If you have an interesting research project fitting to one of the Osteology Foundation grants programmes you are invited to submit your application before June 15, 2015. Detailed information as well as the application guidelines for the research and education grants are available from the Osteology Website. -

Study Protocols: Maxillary Sinus Floor Elevation
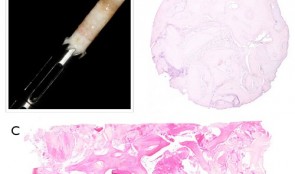
based on the book chapter by Gustavo Avila-Ortiz andPablo Galindo-Moreno Summary This technique is used to gain bone height in posterior atrophic maxillary segments before implant placement. It is increasingly used in patients with maxillary sinuses that are too close to the upper jaw or excessive bone reabsorption from gum disease. Endpoints relate to the amount of new bone formation after grafting and survival of implants and implant-supported prostheses. and long-term success rates are high. It is also excellent for studying healing following grafting with different materials and regenerative strategies in large craniofacial defects. The protocol described here is based on a hypothetical study, and covers patient screening, selection, enrolment and randomization, including a sample size calculation (which is omitted in most published studies). There are multiple phases for planning and executing the sinus elevation, followed by post-operative evaluation, and further planning and placement of implants. Detail is given on the length and form of patient visits for evaluations using cone-beam CT, impressions, photos, clinical measures, bone biopsies and adverse events recording. The discussion is supplemented by images of bone core histology and diagrams of the paranasal sinuses, and the authors point out the difference between crestal and lateral approaches. The lateral approach is illustrated throughout, including follow-up at 24 weeks and implant placement. The authors also address the problems of membrane perforation and nasal meatus occlusion. Open full-text PDF (1.9 MB) -

Study Protocols: Osseointegration Of Dental Implants
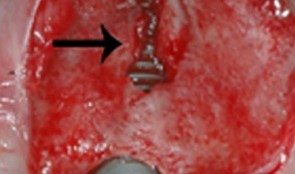
based on the book chapter by Giovanni E. Salvi, Dieter D.Bosshardt, and Niklaus P. Lang Summary The authors explain the rationale behind these techniques and how more in vivo studies of wound healing and tissue formation in humans are needed because most of the existing evidence relates to in vitro animal studies. The protocol has four phases: planning, surgery, laboratory processing and data analysis. It offers an opportunity to obtain standardized, reproducible evidence on the dynamic osseointegration process and allows comparisons to be made between implants with different designs, features and placement sites, for example, and preoperative and postoperative care regimens. It covers enrolment and selection of patients with third molar extractions and good bone volume for undergoing the split-mouth procedure, with details of the healing time points and patient care, and clear images of the procedure. The relevance of implant composition and surface properties (e.g. roughness and wettability) is explained, and the creation of a U-shaped wound compartment in the implant is described, with landmarks that can be identified after explantation. The interface that forms between the implant and bone is evaluated in terms of the bone-to-implant contact (BIC), with endpoints being determined by histology and histomorphometry to reveal immune responses and morphological changes. Microarray gene profiling is used to correlate clinical and molecular events with inflammation, angiogenesis and neurogenesis. The authors remind investigators to engage a biostatistician at an early stage. Open full-text PDF (1.3 MB) -


Study Protocols: Treatment Of Peri-Implantitis
based on the book chapter by Suzanne Mason, Feng Wang, andDarnell Kaigler Summary Treatment of peri-implantitis is a growing area of practice that would benefit from evidence gained from reproducible studies following a standardized protocol. The protocol described here allows evaluation of the effectiveness of anti-infective surgical procedures and interventions through prospective case series and randomized controlled trials. It can be used to study the nature of implantitis, bacterial plaque formation or compare different implant devices. The research question, timeline and patient care routine are specified, with advice on the baseline characteristics, bone loss thresholds and peri-implant probing. Patient eligibility criteria include defined bone loss thresholds and probing depth associated with suppuration or bleeding. The timeline covers recruitment, screening, baseline measurements and treatment, and follow-up of 12 months, with 5 years required to monitor reoccurrences. The cause-related interventions are either non-surgical, using debridement with or without antimicrobial treatment, or surgical, involving mucoperiosteal flap elevation, removal of granulation issue, defect assessment, decontamination of the implant surface and stabilization of defects using bone substitutes, grafts or bioactive substances. The postoperative antimicrobial care regimen involves maintenance care over several months. The authors emphasize the need for calibration of the force of probing and choice of instruments such as a paralleling device for standardizing radiographs. Open full-text PDF (1.3 MB) -


Study Protocols: Regeneration Of Keratinized Gingiva
based on the book chapter by Michael K. McGuire Summary There is an extensive body of evidence relating to soft tissue keratinization and the mucogingival junction (MGJ). This chapter provides an overview of the subject, and revisits the anatomy of the tooth periodontium. The protocol it describes is a randomized trial that targets patients with two non-adjacent sites of one to four tooth spans and less than 2mm of keratinized gingiva. The pre-surgical phases include screening and baseline observations, and the procedure involves comparing an apically positioned flap plus vestibuloplasty (benchmark treatment) with a new therapy. The protocol describes preferred techniques for probing and taking punch biopsies, and specifies dimensions of the wound bed. The authors recommend removing existing keratinized gingiva from the mucosal flaps so that results with the gingival graft are more discernible. They give specific instructions on the method of taking clinical photos. Post-surgical evaluations take place over 6 months, and include patient-reports of postoperative pain and discomfort at the treatment and harvest sites, with inflammatory assessment by a scoring system and measures of apicocoronal width. Other practical recommendations include the use of probes that are calibrated for studies and a 3-mm biopsy punch for revealing the MGJ, as well as allowing a learning curve for surgical techniques, possible pilot patient procedures, carrying out batch surgeries and pre-study power calculations, and consulting a biostatistician. Open full-text PDF (1.4 MB) -


Study Protocols: Root Coverage Regeneration
based on the book chapter byAnton Sculean and Sofia Aroca Summary This protocol relates to root coverage in cases of gingival recession from trauma or disease. Good results can be obtained with a coronally advanced flap technique coupled with connective tissue grafts, but harvesting the tissue is associated with negative factors. An alternative method is soft tissue grafting as used by this protocol, which compares methods and esthetic outcomes in patients with troublesome single and multiple recessions. The selection criteria are stated clearly for patients with Miller class I, II or III gingival recessions in the maxillary or mandibular arch with apicocoronal extension and a recession depth of more than 2 mm. Recruitment is on a multicenter basis, with stratification and randomization into test and control groups, and restrictions on revealing the type of intervention to the surgeons. There are photographs of test and control sites pre-, intra- and postoperatively and at 12 months. Weekly evaluations are carried out for the first month, with a total of 14 visits over the first year. Follow-up is for 35 years. Percentage root coverage is the primary endpoint, with secondary endpoints including patient-reported pain, root sensitivity, tissue thickness and long-term stability. Potential adverse events are listed together with a grading system to assess them. The authors stress the need for surgeon learning curves and calibration of examiners, techniques and equipment, blinded procedures, and engagement of a statistician. Open full-text PDF (1.4 MB)