-


Immediate Function with NoblePerfect Implants
Nölken, RobertProcedure: - Extraction of upper front teeth not suitable for preservation - Immediate loading of four NobelPerfectTM implants - Intraoperative registration of implant position - Flap-free Vestibular Bone Augmentation - Connective Tissue Graft for Periodontal Regeneration - Immediate Loading of temporary implants on the day of surgery - Definitive restoration 6 months later Materials: NobelPerfect Groovy Implants RP and NP; NobelPerfect Temporary Abutments RP and NP; NobelPerfect Implant Replicas RP and WP; Ribbond, Bondable Reinforcement Ribbon; Ethilon 5-0 FS3 Suture Material; Astra Bonetrap Bone Collector. -


Connective tissue graft for recession defect coverage and vertical osseous defect in the anterior mandible
Heinz, Bernd / Jepsen, SørenContents: 1. Removal of free connective tissue graft from palate 2. Suturing to close graft removal site 3. Making the incision for coronal sliding flap 4. Cleaning and smoothing root surface with instruments 5. Removal of granulation tissue 6. Setting the free connective tissue graft into position 7. Graft fixation 8. Mobilizing the coronal sliding flap 9. Flap fixation -


Access-Flap for Treatment of Aggressive Periodontitis
Beck, FrankContents. Aggressive periodontitis leads to early and extensive loss of periodontal supporting tissue. Controlling the infection is of serious importance to avoid further loss of attachment. The surgical procedure is difficult, especially if the tissue is already severely damaged. The challenge for the surgeon is to protect and conserve the tissue as much as possible. -


The use of autologous PRGF in periodontal plastic surgery
Marggraf, ErwinContents: - Blood sampling - Platelet separation activation - Introduction of bone replacement material - Access flap and curettage - Introduction of PRGF and bone replacement material - Plastic suture Materials Checklist: All materials required for producing PRGF (BTI Germany) Bone replacement materials Geistlich Biomaterials Surgical instruments, Aesculap Suture materials, Ethicon -


Recession coverage using human dermal tissue at site 22-26
Schlee, Markus -

Recession coverage with connective tissue using the envelope technique at site 13
Ratka-Krüger, PetraList of materials: Periodontometer, handle #6 (Hu-Friedy); Universal probe, handle #6 (Hu-Friedy); Mirror handle #6 (Hu-Friedy); Transfer handle, round; Respiratory, Hirschfeld; Surgical curettes, Prichard; Universal curettes, Younger-Good, handle #6; Universal curette, Indiana University, handle #6; Universal curette, Langer After-Five, handle #6; Tweezers, Gerald; Tweezers, fine; Spatula, fine; Tissue cutter, Super-Cut; Thread cutter, Godman-Fox; Needle holder, Lichtenberg; Needle holder, Castroviejo; Hemostat; Scalpel blades; Tunneling instruments; Gingivectomy meter, Orban, handle #6; Blade holder, Universal 360°; Suture material, polypropylene C6; Suture material, polypropylene C17. -


Proceedings of the 2014 AAP Regeneration Workshop
AAP & Osteology FoundationOn June 1-4, 2014 the AAP organised an international consensus workshop, co-chaired by the Osteology Board members William V. Giannobile and Pamela K. McClain. The workshop was of huge interest to the Osteology Foundation and therefore supported with an educational grant. The proceedings of this workshop are available with free access in a special supplement of the Journal of Periodontology: -

-

-
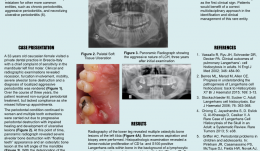

THE ROLE OF MULTIDISCIPLINARY APPROACH IN A CASE OF LANGERHANS CELL HISTIOCYTOSIS WITH INITIAL PERIODONTAL MANIFESTATIONS
Objectives: The present case epitomizes the clinical situation of a single-system Langerhans cell histiocytosis (LCH) mimicking aggressive periodontitis in a patient with no other clinical signs. Although this is a single observation, we highlight the importance of using a multidisciplinary approach in rare conditions like this for optimizing patient management. Methods: A 32-year-old Caucasian woman visited a private dental practice in Brescia, Italy, complaining of sensitivity in her mandibular left first molar. Clinical and radiographic examinations revealed recession, furcation involvement, mobility and severe alveolar bone loss, leading to a diagnosis of localised aggressive periodontitis. Over the next 3 years, the patient received non-surgical periodontal treatment, but failed attend successive follow-up appointments for undisclosed reasons. Her periodontal condition continued to worsen and multiple tooth extractions were carried out due to progressive periodontal destruction with impaired healing and development of ulcerative lesions. Panoramic radiographs were taken, and revealed severe alveolar bone destruction with “floating teeth” appearance, and an osteolytic bone lesion at the left angle of the mandible. With an overall clinical deterioration, and the possibility of an underlying malignant condition, the patient was referred for deep analysis. Results: No abnormalities were detected in laboratory and biochemical tests. Skull and sinus radiography revealed a 5-mm oval radiolucency at the left angle of the mandible. Then a radiograph of the lower leg revealed multiple osteolytic bone lesions of the left tibia. Bone-marrow aspiration and biopsy were performed to determine the nature of these lesions. Histopathology revealed a dense nodular proliferation of CD1a-positive and S100-positive Langerhans cells within bone, on a background of lymphocytic and granulocytic cells, consistent with LCH. An additional biopsy of the intra-oral lesion showed mature, disease-free, compact bone. However, a bone biopsy may be not representative of the entire structure, particularly in cases of intraoral localisation of LCH. Bidirectional Sanger sequencing analysis and pyrosequencing of DNA extracted from bone tissue of the tibia detected the presence of the BRAF-V600E hotspot somatic mutation, confirming a clonal origin of the neoplastic cells. Multidisciplinary investigations showed that the periodontal involvement was a manifestation of an underlying systemic disease (multifocal single-system LCH). The patient was then started on radiotherapy and but improvement of her oral and periodontal condition is yet to be confirmed. Conclusions: In the present case, LCH was unrecognised for several years. The periodontal disease progressed rapidly, leading to loss of most of the dentition, with persistent delays in soft tissues healing after extraction. Close monitoring of the oral signs may have allowed earlier diagnosis of LCH and prevent such rapid deterioration, possibly resulting in a better endpoint. Dentists and periodontists should be aware that rare systemic diseases such as LCH can produce oral manifestations as the first clinical sign. Such patients benefit from a multidisciplinary approach to identify and manage such entities. -


AAP Collaboration: Workshop Proceedings published
Enhancing Periodontal Health Through Regenerative Procedures Fifty-two workshop participants met in Chicago last summer to conduct a systematic review of existing literature, culminating in the development of consensus reports and practical applications to aid practitioners in the clinical environment. Topics of the workshop included the following: Periodontal Soft Tissue Root Coverage Procedures: Managing gingival recession based on current evidence with a primary outcome goal of complete root coverage Periodontal Soft Tissue Non-Root Coverage Procedures: Assessing the need for gingival augmentation procedures (non-root coverage) around natural teeth Intrabony Defects: Periodontal regenerative strategies for the management of intrabony periodontal defects Furcation Defects: How periodontal furcation defects should be managed via periodontal regenerative therapy and what parameters should be used for treatment selection Emerging Regenerative Approaches for Periodontal Reconstruction: Can emerging technologies for periodontal regeneration become clinical reality? Each practical applications paper describes a specific clinical situation, different approaches that may be considered in its management, and how an expert makes a treatment decision based on the provided evidence. Clinical Advances in Periodontics also offers illustrative images and videos that further detail the clinical situation, how it was managed, and its expected treatment outcomes. How the workshop came to be and what the findings mean for periodontal practice The2014 AAP Regeneration Workshopon the topic Enhancing Periodontal Health Through Regenerative Procedures was of huge interest to the Osteology Foundation, and therefore it was supported with an educational grant. The international consensus meetingwas co-chaired by theOsteology BoardmembersWilliam V. GiannobileandPamela K. McClain. We are excited to announce that the proceedings of this workshop have now been published in a special supplement of the Journal of Periodontology, and are available online with free access. Proceedings of the 2014 AAP Regeneration Workshop The publication is a great result of the first joined efforts of the AAP and the Osteology Foundation. The results havedemonstrated that regenerative procedures are effective and predictable treatment options for helping patients retain their natural dentition. The workshop was an amazing collaborative effort that provides the most current consensus of therapies and technologies in regenerative treatment, sayd AAP president Joan Otomo-Corgel at a press-conference in Chicago, when the publication was announced. Were thrilled to share the results of the these dynamic discussions. This bell weather information will provide tremendous benefit to the periodontal specialty, the dental community, and the patients we treat. -














